How Serious is a Nodule on the Liver? What You Need to Know
 Written By
Jaclyn P. Leyson-Azuela, RMT, MD, MPH
Written By
Jaclyn P. Leyson-Azuela, RMT, MD, MPH
A nodule on the liver can be a worrisome finding. But the question “how serious is a nodule on the liver” depends on several factors like its size, appearance, and whether the nodule is benign or malignant. Many liver nodules are noncancerous and cause no symptoms at all. In fact, many of these are only found by chance when you undergo scanning for a different medical reason.
However, other nodules could indicate underlying liver disease or even liver cancer. Accurate diagnosis through imaging tests and, in other cases, biopsy is an important step to determine what’s causing the nodule. It could also guide appropriate management plans. Understanding the seriousness of the nodule on the liver is important for timely and effective medical treatment.
Key Takeaways
-
Most liver nodules are benign and don’t require treatment
-
Size matters — nodules larger than 5 cm have higher chance of being cancerous
-
In patients with indeterminate nodules, the incidence of hepatocellular carcinoma increases to 30% over time.
-
Having cirrhosis increases the likelihood of a nodule being cancerous with 8.3% cumulative risk
-
There are warning signs you should watch out for like nodule growth, specific imaging features, and symptoms, such as jaundice or right upper abdominal pain
-
Treatment options range from simple watchful waiting for benign growth to surgery for cancerous nodules
What is a Liver Nodule?

A liver nodule pertains to a small lump or growth that develops in your liver tissue. These lumps can range from a very small (<1 cm) to several centimeters in diameter. Many people have them without even knowing they exist throughout their lifetime.
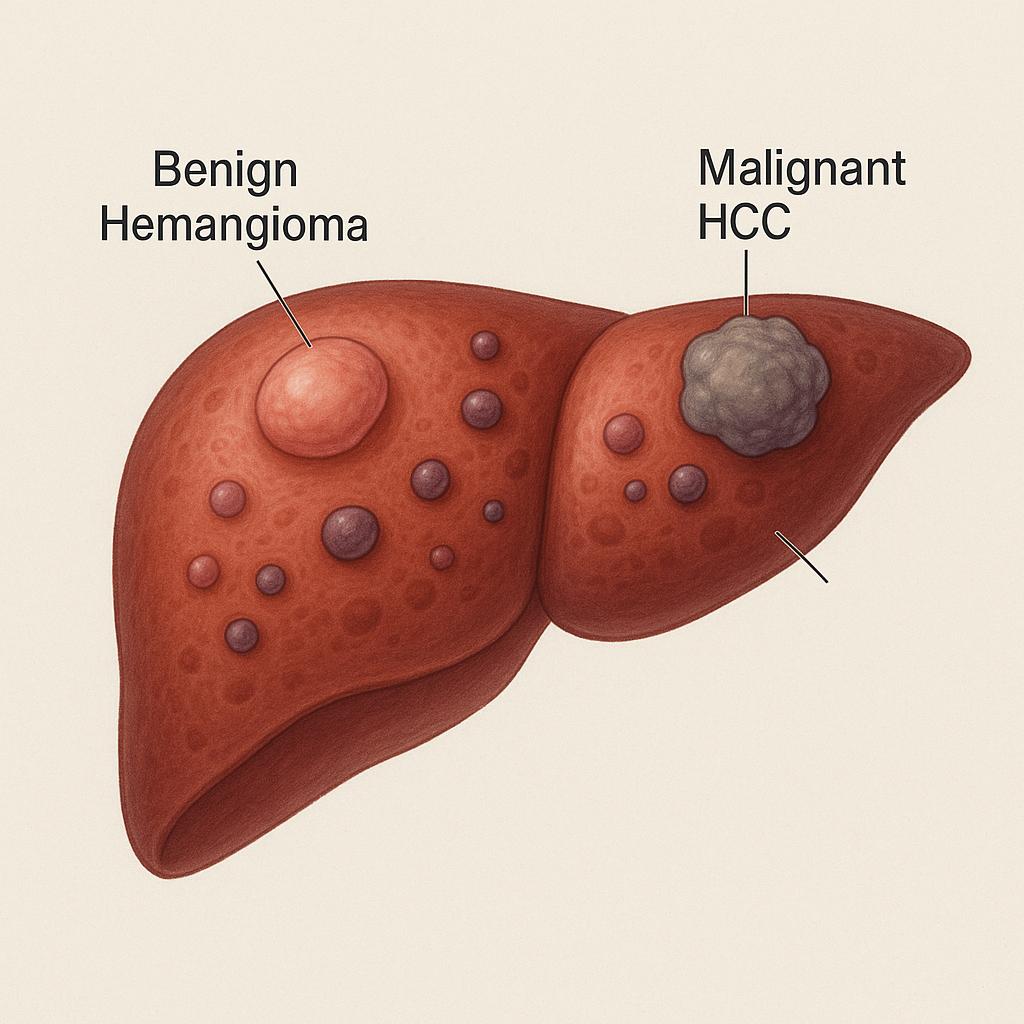
Liver nodules come in different types. Some of them are completely harmless (benign), while others can be harmful (malignant).
Benign Liver Nodules:
Most liver nodules are benign and do not carry risks to health. Common types include:
-
Hemangiomas (most common): These are blood vessels clumped together.
-
Focal nodular hyperplasia (FNH): An overgrowth of normal liver tissue with a star-shaped appearance on its center.
-
Hepatic adenomas: Rare nodules frequently related to intake of oral contraceptive pills
-
Cysts: Fluid-filled sacs
-
Lipomas: Nodules composed of fat
These nodules are discovered incidentally during scanning for different medical reasons since they do not cause symptoms (or rarely if at all). But if they grow large and push on other tissues, it may cause some discomfort.
Hepatic adenomas carry a risk of bleeding or transforming into liver cancer. So it may need to be periodically monitored or surgically removed if large, causing symptoms, or has features that suggest cancer risk.
Malignant Liver Nodules:
These nodules are malignant (cancerous) and carry with them significant risks. Most common primary liver cancers include:
-
Hepatocellular carcinoma (HCC): The most common type of liver cancer.
-
Cholangiocarcinoma: Type of nodule that starts in the bile ducts.
-
Metastases: A type of cancer that has spread to the liver from other parts of the body
Quick Overview of Benign vs Malignant Nodules
|
Feature |
Benign Nodules |
Malignant Nodules |
|
Cancer risk |
None or very low (except some adenomas) |
High |
|
Symptoms |
Usually none; pain if they are large |
May cause pain, weight loss, jaundice |
|
Treatment |
Often none; surgery if they are large or symptomatic |
Requires cancer therapy (surgery, chemo, etc.) |
|
Follow-up |
Sometimes needed if there is risk of growth/bleeding |
Intensive monitoring and treatment |
|
Risk factors |
Rarely related to underlying liver disease |
Cirrhosis, hepatitis B/C, cancer elsewhere |
What Causes Liver Nodules?
There are several things that may cause liver nodules to develop. One of the major culprits is infection with Hepatitis B and C. These viruses attack your liver cells, which then cause damage and result in nodule formation. About 70% of liver cancer cases come from these infections.
Heavy alcohol use is another major cause. When you drink too much, your liver gets inflamed. Once the inflammation resolves, the damage is not reversed, resulting in scarring of the liver tissue. The damage from this could lead to the development of nodules. And, around 35-45% of liver cancer cases are attributed to alcohol abuse.
Non-alcoholic fatty liver disease (NAFLD) occurs when excess fat accumulates in your liver. Around 25% (100 million) of Americans have this condition and some of these patients develop nodules because of this. And, they may not know it!
Genetics can play a huge part too. Some people may inherit conditions that will increase their likelihood of developing liver nodules. Examples of these conditions, include:
-
Hemochromatosis (too much iron)
-
Wilson’s disease (too much copper)
Other causes for liver nodule to occur include:
-
Certain medications
-
Autoimmune diseases
-
Exposure to toxins
-
Diabetes
-
Obesity
Different types of nodules also have different causes. As mentioned, HCC (liver cancer) is strongly associated with cirrhosis.
Are All Liver Nodules Serious?
Fortunately, most liver nodules are not serious and are benign even in patients with liver cirrhosis. However, some of these cases have the potential to become malignant over time.
The key here is telling the difference between what’s harmful and what you can ignore. There are specific factors that will tell doctors clues, which they will use to decide whether the nodule is a cause of worry:
-
Size matters — nodules larger than 5 cm or about 2 inches have higher chance of being cancerous
-
Growth patterns — if a nodule grows quickly, this needs more attention. Nodules with a growth rate of more than 50% in just six months is the threshold, which raises red flags for cancer.
-
Symptoms are warning signs — benign nodules often cause no symptoms. In fact, most of them are just discovered incidentally (which are found in imaging not intended to find them). However, it raises suspicion if you have the following:
-
Right upper abdominal pain
-
Unintentional weight loss
-
Jaundice (yellow discoloration of skin and eyes)
-
Having cirrhosis also increases the likelihood of a nodule being cancerous with 8.3% cumulative risk
These are the reasons why doctors often monitor patients closely. Your liver blood tests can offer some clues to the diagnosis too. If you have abnormal results in your liver function tests or other liver laboratory work-up, it may suggest that the nodule is affecting how your liver functions.
Can Liver Nodules Become Cancerous?
Yes. Liver nodules can be cancerous or become one, if the circumstances allow it to be. The most common type of liver cancer is HCC as mentioned and it starts in the hepatocytes (main liver cells). People with cirrhosis face particularly the highest risk — at about 80-90% risk to develop HCC.
Fortunately, treatment for liver cancer works best if it’s found early. The definition for early stage varies by the staging system used. But using the most widely used method — the Barcelona Clinic Liver Cancer (BCLC), it defined staging in two distinct cases:
-
Very early stage as a nodule that’s single, measuring less than 2 cm without derangement in liver function and performance status
-
Early stage is defined as a nodule that’s single or less than 3 nodules, each with less than 3 cm in diameter without derangement in liver function and performance status
Having defined that, a very early stage HCC that is less than 2 cm in diameter has a 5-year survival rate of 65-70%. The rate decreases to 50% if the tumor size is at 2-5 cm in diameter.
How Are Liver Nodules Diagnosed?

Identifying and looking for a liver nodule may require using multiple diagnostic approaches.
The majority of the liver nodules are found by accident, especially if you undergo imaging for some other medical reasons. Nonetheless, the following are the diagnostic modalities being used:
-
Ultrasound is usually the first test. It uses sound waves to create images of your liver. It is easily accessible, painless, no radiation, and is great at screening for nodules. But ultrasound may miss small nodules and doesn’t always tell whether the nodules are malignant or benign.
-
Computed tomography (CT) scans take images of the liver from different angles. They’re excellent at finding smaller nodules and can give more details about the features of the nodules. It has a sensitivity of 33-45% and specificity of 33-67% for smaller nodules.
-
Magnetic resonance imaging (MRI) gives the most detail when it comes to liver nodules. It uses magnetic fields instead of radiation. It can demonstrate subtle differences between tissues. MRI has a sensitivity of 44% for nodules that are between 1-2 cm. It is also great at demonstrating blood flow patterns that help detect HCC. To improve detection, liver-specific contrast agents may be used. The contrast (dye) agents are taken up by normal liver tissue cells but not by cancer cells. This makes the detection of cancerous nodules easier.
-
Biopsy (taking a tissue sample) is the gold standard for confirming the presence of HCC. The tissue sample is sent to the laboratory and examined under the microscope. This carries some risks like bleeding.
There are laboratory tests that can help too, such as:
-
Alpha-fetoprotein (AFP) is a marker that increases when HCC is present. However, studies have shown that as high as 40% of HCC cases have normal AFP levels.
When ultrasound is combined with AFP, the ability to diagnose HCC reaches more than 90%.
What Makes a Liver Nodule Serious?
There are telltale signs that tell if a liver nodule needs immediate medical care. These are usually the red flags for that particular nodule:
-
Size and growth rate. Size alone is not a predictor that the liver nodule is serious. Rather, its ability to reach a certain size at a faster rate is indication that the nodule needs testing and attention.
-
Imaging characteristics. The cancerous nodules often show a pattern called “washout” on CT or MRI scans. This term is used to describe how the nodule takes up the dye then fades faster than the rest of the liver. This pattern is the imaging hallmark feature of HCC.
-
Symptoms. Benign nodules (except those large enough to press on surrounding tissues) often don’t cause symptoms. But if they do, you need to be wary of the following symptoms:
-
Upper right abdominal pain
-
Unexplained weight loss
-
Bloating or feeling full quickly when eating
-
Jaundice (yellowing of the skin or eyes)
-
Swelling in the abdomen
-
Location of the nodule. Nodules that are located near major blood vessels may be harder to treat and could suggest that they are aggressive.
The symptoms may indicate some serious liver problem like cirrhosis of the liver. If you have cirrhosis and a finding of liver nodule, it is likely that your doctor will press for more investigation.
Multiple nodules seen in the liver may suggest metastases from a primary cancer that’s from other parts of the body. However, without confirmatory tests, multiple small nodules can be caused by benign conditions like hemangiomatosis.
High levels of AFP in blood tests could also raise concern. Generally, the normal value for AFP is less than 10 ng/mL. AFP levels reaching more than 400 ng/mL strongly indicate that the liver nodule may be HCC.
How is a Liver Nodule Treated?
The treatment for liver nodules follows a case-to-case basis. The plan depends on the type of nodule you have.
-
For benign nodules, watchful waiting and periodic monitoring is often enough. What doctors do in these instances may include regular imaging every 3-6 months to ensure that the size of the nodule is stable as well as its characteristics.
-
Hemangiomas and FNH require no treatment except when they cause symptoms.
-
Adenomas carry a small risk of bleeding or becoming cancerous. The recommendation would be:
-
To stop taking birth control pills (which makes these nodules grow)
-
Undergo surgery for removal of larger nodules larger than 5 cm
-
Make lifestyle changes like losing weight
-
For malignant nodules, the treatment options include:
-
Surgery (resection) to remove the nodule and a significant margin on its surrounding tissue. This is usually done for cancers that are localized or have not spread yet. Early-stage HCC surgery has a 5-year survival rate of nearly 60%.
-
Liver transplantation is another treatment option that will replace the diseased liver. It is reserved for patients with cirrhosis and early-stage HCC. The 5-year survival rate of these patients reaches as high as 60-70%.
-
Ablation is a form of treatment that destroys the nodule without removing it. It includes the following options:
-
Radiofrequency ablation (RFA) — uses heat from electrical currents
-
Microwave ablation — uses heat from microwave energy
-
Cryoablation — uses freezing and kill cancer cells
-
Alcohol injection — injects pure alcohol directly to the nodule
-
Embolization is a method to cut off the blood supply of the tumor. It includes the following:
-
Transarterial chemoembolization (TACE) — delivers chemotherapy directly to the tumor along with agents that block its blood supply
-
Radioembolization — uses radioactive beads that target tumors
-
Radiation therapy uses high-energy rays to kill cancer cells
-
Stereotactic body radiation therapy (SBRT) is a new technique that targets specifically the liver tumors
-
Systemic treatments include:
-
Targeted therapy drugs
-
Immunotherapy
The treatment options vary considerably by nodule type, location, size, and your overall health.
What to Do if You Have a Liver Nodule?

Finding out that you have a liver nodule may be a cause of worry. But knowing what to do can make a difference. So what do you do if you find out you have a liver nodule?
-
Consult your primary care doctor and follow the recommendations. If they advise that you undergo periodic monitoring, don’t skip any of these appointments. These check-ups allow you to know whether the nodules are stable over time, which says a lot about the properties of the liver nodule.
-
Ask your doctor specific questions like what is the specific nodule type you have. Have your healthcare provider explain what it means and what you can do moving forward.
-
Adopt a healthy lifestyle and let go of bad habits to ensure optimal liver function and health.
-
Eat balanced and nutritious food
-
Stay away from sugary and processed foods, and those with high saturated fats
-
Maintain a healthy weight
-
Exercise religiously (150 minutes of moderate activity each week can’t hurt)
-
Avoid if not stop consuming alcohol
-
Don’t take medications, you don’t need or without consulting your doctor first
-
Get vaccinated against hepatitis A and B
-
Know when to call for help right away

Call your doctor if you have the following:
-
Increasingly painful right upper abdomen
-
New or worsening abdominal swelling
-
Jaundice
-
Unusual fatigue that is not relieved with rest
-
Unintentional weight loss
Conclusion
Many people with liver nodules live long, high-quality lives by staying proactive and participative in keeping their liver health. Most of these nodules are benign and usually won’t need intervention or immediate management. However, if you have the risk factors (e.g., cirrhosis), these nodules have an increased risk of becoming cancerous. By learning how to differentiate how serious is a nodule on the liver, you are empowered to move forward with a plan and ensure your health in the following years.
If you want to start monitoring your liver health, Ribbon Checkup has a way of getting this done right at the comforts of your own home.
References
Asafo-Agyei, K. O., & Samant, H. (2023). Hepatocellular carcinoma. PubMed; StatPearls Publishing. https://www.ncbi.nlm.nih.gov/books/NBK559177/
Bengtsson, B., Widman, L., Renumathy Dhanasekaran, Per Stål, Björkström, N. K., & Hannes Hagström. (2022). The risk of hepatocellular carcinoma in cirrhosis differs by etiology, age and sex: A Swedish nationwide population‐based cohort study. 10(5), 465–476. https://doi.org/10.1002/ueg2.12238
Bialecki, E. S., & Di Bisceglie, A. M. (2005). Diagnosis of hepatocellular carcinoma. HPB, 7(1), 26–34. https://doi.org/10.1080/13651820410024049
Charifa, A., Azmat, C. E., & Badri, T. (2020). Lipomas, Pathology. PubMed; StatPearls Publishing. https://www.ncbi.nlm.nih.gov/books/NBK482343/
Garikipati, S. C., & Roy, P. (2020). Biliary Tract Cholangiocarcinoma. PubMed; StatPearls Publishing. https://www.ncbi.nlm.nih.gov/books/NBK560708/
Hsee, L., McCall, J. L., & Koea, J. (2005). Focal nodular hyperplasia: what are the indications for resection? Hpb, 7(4), 298–302. https://doi.org/10.1080/13651820500273624
Jeon, Y., Choi, Y. S., Jang, E. S., Kim, J. W., & Jeong, S.-H. (2017). Persistent α-Fetoprotein Elevation in Healthy Adults and Mutational Analysis of α-Fetoprotein Promoter, Enhancer, and Silencer Regions. Gut and Liver, 11(1), 136–141. https://doi.org/10.5009/gnl16069
Ju, M. R., & Yopp, A. C. (2021). Surgical resection of early stage hepatocellular carcinoma: balancing tumor biology with the host liver. Chinese Clinical Oncology, 10(1), 5. https://doi.org/10.21037/cco-20-130
Lachance, E., Mandziuk, J., Sergi, C. M., Bateman, J., & Low, G. (2021). Radiologic-Pathologic Correlation of Liver Tumors. Liver Cancer, 87–108. https://doi.org/10.36255/exonpublications.livercancer.2021.ch5
Lee, C.-W., Tsai, H.-I., Lee, W.-C., Huang, S.-W., Lin, C.-Y., Hsieh, Y.-C., Kuo, T., Chen, C.-W., & Yu, M.-C. (2019). Normal Alpha-Fetoprotein Hepatocellular Carcinoma: Are They Really Normal? Journal of Clinical Medicine, 8(10), 1736. https://doi.org/10.3390/jcm8101736
Lee, W.-C. (2021). Value of alpha-fetoprotein in hepatocellular carcinoma. Translational Gastroenterology and Hepatology, 6, 52–52. https://doi.org/10.21037/tgh.2019.12.19
Liver Cancer Survival Rates | Cancer of the Liver Survival Rates. (n.d.). Www.cancer.org. https://www.cancer.org/cancer/types/liver-cancer/detection-diagnosis-staging/survival-rates.html
Liver Lesions: Types, Causes, Symptoms & Treatment. (2021, May 18). Cleveland Clinic. https://my.clevelandclinic.org/health/diseases/14628-liver-lesions
Nonalcoholic Fatty Liver Disease (NAFLD). (2025, February 13). American Liver Foundation. https://liverfoundation.org/liver-diseases/fatty-liver-disease/nonalcoholic-fatty-liver-disease-nafld/
Pinter, M., Trauner, M., Peck-Radosavljevic, M., & Sieghart, W. (2016). Cancer and liver cirrhosis: implications on prognosis and management. ESMO Open, 1(2), e000042. https://doi.org/10.1136/esmoopen-2016-000042
Rao, P. N. (2014). Nodule in Liver: Investigations, Differential Diagnosis and Follow-up. Journal of Clinical and Experimental Hepatology, 4, S57–S62. https://doi.org/10.1016/j.jceh.2014.06.010
Shreenath, A. P., & Kahloon, A. (2020). Hepatic Adenoma. PubMed; StatPearls Publishing. https://www.ncbi.nlm.nih.gov/books/NBK513264/
Testino, G., Leone, S., & Borro, P. (2014). Alcohol and hepatocellular carcinoma: A review and a point of view. World Journal of Gastroenterology : WJG, 20(43), 15943–15954. https://doi.org/10.3748/wjg.v20.i43.15943
Yahia, Y., Qasem, M., Abbarh, S., Saffo, H., Obeidat, I. M., Barjas, H. H., Faisal, M. M., Halabiya, M., Chandra, P., & Derbala, M. (2024). Risk of Malignancy in Indeterminate Liver Nodules Among Patients with Cirrhosis: A Retrospective Cohort Study. Journal of Gastrointestinal Cancer, 56(1). https://doi.org/10.1007/s12029-024-01122-7
Yoon, J. H., & Choi, S. K. (2023). Management of early-stage hepatocellular carcinoma: challenges and strategies for optimal outcomes. Journal of Liver Cancer, 23(2), 300–315. https://doi.org/10.17998/jlc.2023.08.27

Jaclyn P. Leyson-Azuela, RMT, MD, MPH, is a licensed General Practitioner and Public Health Expert. She currently serves as a physician in private practice, combining clinical care with her passion for preventive health and community wellness.



