Liver Failure Death Timeline: Understanding What This Means
 Written By
Jaclyn P. Leyson-Azuela, RMT, MD, MPH
Written By
Jaclyn P. Leyson-Azuela, RMT, MD, MPH
Liver failure death timeline varies from sudden acute cases to gradual chronic progression over the years. The progression depends on whether you're dealing with acute or chronic liver failure, with outcomes ranging dramatically based on early intervention and treatment access.
Research shows that from 1999-2016 cirrhosis-related deaths increased by up to 65%. So liver failure death timeline is very crucial to understand for patients and families. Acute liver failure can progress to death without immediate medical intervention. Chronic liver failure, on the other hand, typically develops over months to years through distinct stages.
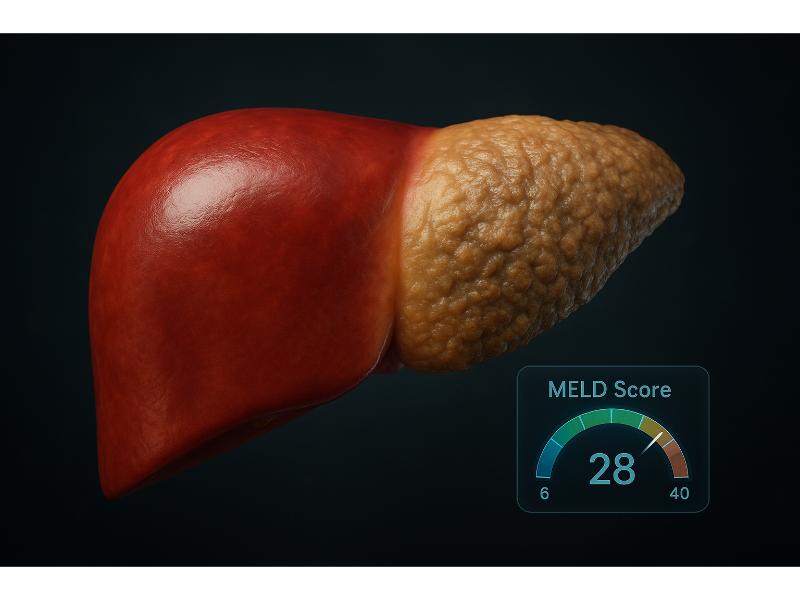
The MELD (Model for End-Stage Liver Disease) score helps your doctor predict survival rates. Scores above 40 indicate extremely high death risk within months. But modern treatments including liver transplantation have significantly improved outcomes. Acute liver failure cases had a 1-year survival rate of more than 65% with proper care and management.
Key Insights
-
Acute can lead to death in days without treatment, while chronic progresses over years through stages like cirrhosis
-
Decompensated cirrhosis has ~50% two-year survival; acute improved to more than 65% 1-year survival with modern care
-
Symptoms of end-stage liver disease include jaundice, ascites, encephalopathy signal poor prognosis, which often require palliative support
-
Linked to alcohol, obesity; early detection via lab tests crucial for better outcomes
-
Lifestyle changes, medications, transplants; palliative care improves quality in final phases
What Causes Liver Failure?
Liver failure stems from acute triggers like drug overdose or chronic conditions like alcohol abuse that directly impacts death timelines from days to years. Knowing the underlying cause helps predict progression speed and treatment options.
Acetaminophen overdose remains the leading cause of acute liver failure, which accounts for about 50% of liver failure cases in the US and 20% of liver transplant cases. Causes of acute liver failure can overwhelm the liver’s regenerative capacity within hours to days. On the other hand, chronic liver failure cases develop slowly, allowing the liver to compensate until the later stages.
What Are Common Causes of Acute Liver Failure?
Acute liver failure develops rapidly, often within but less than 26 weeks of symptom onset, with specific triggers requiring immediate medical attention.
-
Acetaminophen toxicity
-
Drug-induced liver injury (including prescription medications and herbal supplements)
-
Viral hepatitis (hepatitis A, B, C, and rarely E)
-
Autoimmune hepatitis
-
Wilson’s disease (copper accumulation)
Modern emergency interventions have improved 21-day survival rates to approximately 75% since 1998. This is especially true when patients have access to specialized care at liver transplant centers.
What Are Common Causes of Chronic Liver Failure?
Chronic liver failure develops over the years through continuous and repeated liver damage. The current trend in the US shows increased correlation of chronic liver failure with alcohol consumption and obesity.
-
Alcohol-related liver disease affects about 1 in 20 adults in the US
-
Non-alcoholic fatty liver disease (NAFLD, now known as MASLD or metabolic-dysfunction associated steatotic liver disease) affects roughly 25% of the global population
-
Chronic hepatitis B and C viral infections cause long-term inflammation
-
Autoimmune conditions like primary biliary cholangitis and sclerosing cholangitis
-
Metabolic disorders, such as alpha-1 antitrypsin deficiency and hemochromatosis
Regular laboratory monitoring can detect progression only. This allows interventions that may slow or halt disease advancement before irreversible damage occurs.
What Are the Stages of Liver Failure?
Liver failure progresses through inflammation, fibrosis, cirrhosis, and eventually end-stage liver disease. The timeline could span months to decades depending on the treatment and management. Acute cases mostly skip the gradual stages and progress so fast to liver failure.
Understanding these stages helps patients recognize when medical intervention becomes critical. Each of these stages represent increasing liver damage, though early stages remain potentially reversible with the right treatment and lifestyle modifications.
The Child-Turcotte-Pugh (CTP) classification system provides the grading system for the severity of cirrhosis from Class A (best outcome) to Class C (poorest outcome). This classification system allows prediction of liver failure death timeline and treatment urgency.
What Happens in Stage 1: Inflammation?
Stage 1 involves reversible liver swelling from injury or infection. This typically lasts weeks when properly treated.
During this initial stage, the liver becomes inflamed as immune cells respond to damage. Symptoms may include:
-
Mild upper right abdominal discomfort or dull pain
-
Elevated liver enzyme levels on blood tests
-
Occasional fatigue or weakness
-
Normal liver function despite inflammation
If it is caused by viral hepatitis, the recommendation is to initiate immediate antiviral therapy to mitigate the inflammation and may even fully resolve the condition especially when caught early. Liver inflammation responds well to removing the underlying cause or trigger, whether it’s abstinence from alcohol, medication changes, or viral treatment.
What Happens in Stage 2: Fibrosis?
Stage 2 features scar tissue buildup that often remains asymptomatic or without symptoms for years. But it can be detected through specialized testing.
Scar tissue formation occurs as the liver attempts to heal from the repeated injury. The characteristics of this stage, include:
-
Progressive scarring visible on imaging studies
-
Generally preserved liver function initially
-
Detection possible through FibroScan technology available
-
Potential reversibility with aggressive treatment of underlying causes
Monitoring through specialized laboratory tests can help track the status of fibrosis progression. It will also allow timely interventions before permanent damage develops.
What Happens in Stage 3: Cirrhosis?

Stage 3 cirrhosis is divided into:
-
Compensated phase (median survival of 12 years)
-
Decompensated phase (median survival of 2 years)
Compensated cirrhosis maintains enough liver function despite the presence of extensive scarring. Decompensated cirrhosis occurs when the liver no longer performs its essential functions.
Key differences include:
|
Compensated Cirrhosis |
Decompensated Cirrhosis |
|
CTP Class A: ~100% one-year survival rate |
CTP Class C: 45% one-year survival rate |
|
Often asymptomatic for years |
Development of ascites, portal hypertension, or encephalopathy |
|
Regular monitoring prevents complications |
Requires immediate transplant evaluation |
What Happens in Stage 4: End-Stage Liver Disease?
Stage 4 represents complete liver failure with survival timelines measured in months without transplantation. It is often associated with sudden death risk.
End-stage symptoms indicate imminent liver failure requiring palliative care consultation:
-
MELD scores exceeding 40 indicate extremely poor prognosis
-
Multiple organ system involvement becomes common
-
Hepatic encephalopathy affects cognitive function
-
Kidney failure develops in approximately 10% of patients
Mortality timeline in this stage varies from weeks to several months, with sudden death possible from complications like gastrointestinal bleeding or even severe infections.
How Long Can You Live with Liver Failure?

Survival with liver failure ranges from days to weeks in acute cases to 2-12 years in chronic conditions. It is primarily determined by disease stage and access to treatment. Modern medical advances have significantly improved the outcomes, particularly in patients receiving timely and specialized intervention.
Statistics show that decompensated liver cirrhosis shows only about 45% one-year survival rate. Acute status of liver failure has a higher survival rate if timely and correct interventions are initiated in specialized centers. Liver transplantation dramatically improves patient outcomes.
Age, overall health status, and underlying liver disease significantly influence survival projections, with younger patients generally experiencing better outcomes across all categories.
What Are Survival Rates for Acute Liver Failure?
As mentioned earlier, acute liver failure achieves 75% 21-day survival rates with modern intensive care, representing substantial improvements since 1998.
Factors affecting the survival rates in acute cases include:
-
Timely or immediate medical intervention
-
Transplant availability
-
Age and health status
-
Cause of failure
Specialized liver failure units achieve significantly better outcomes than general intensive care settings.
What Are Survival Rates for Chronic Liver Failure?
Also mentioned earlier, chronic liver failure survival correlates directly with CTP classification, ranging from excellent prognosis in early stages to urgent transplant needs in advanced cases.
CTP Classification Survival Rates:
-
Class A (early): Nearly 100% one-year survival
-
Class B (moderate): 80% one-year survival
-
Class C (severe): 45% one-year survival
The transplantation waitlist varies significantly by geographic region. As a result, it affects access to life-saving procedures. Patients in certain regions may wait months or even longer than other regions before they can get suitable donor organs.
What Are the Symptoms of End-Stage Liver Failure?
End-stage liver failure symptoms include:
-
Jaundice
-
Ascites
-
Confusion or disorientation
When these symptoms appear, it may only take weeks to months remaining before death. In about 60% of patients within this stage, significant pain is experienced that often requires specialized management approaches.
Hepatic encephalopathy affects daily functioning and independence, often becoming the most distressing symptom for families. These neurological changes indicate toxin buildup that the failing liver cannot process effectively.
Physical symptoms progress predictably, helping healthcare teams provide appropriate supportive care and realistic timeline expectations for patients and families.
What Are Physical Symptoms in End-Stage Liver Failure?
Physical manifestations include jaundice, abdominal swelling, and upper right abdominal pain, with ascites developing in 73% of patients.
In detail, primary physical symptoms in end-stage liver failure, include:
-
Yellow discoloration of skin, eyes, and mucosa due to bilirubin buildup (which you may also check for its metabolite urobilinogen in at-home urine testing)
-
Ascites is the buildup of fluid in the abdomen, which often requires diuretic management
-
Edema of the ankles and legs, often from protein deficiency
-
Spider angiomata is a cluster of small blood vessels on the chests and arms
-
Esophageal varices are dangerously enlarged veins that are prone to bleeding
Diuretic protocols help manage fluid retention, though effectiveness decreases as liver function deteriorates further.
What Are Neurological Symptoms in End-Stage Liver Failure?
Hepatic encephalopathy affects brain function when the failing liver cannot remove toxins, significantly impacting 12-month survival rates.
Neurological progression includes:
-
Mild confusion or difficulty in concentration and memory
-
Sleep pattern disruption, often reversal of day-night cycles
-
Personality changes, such as irritability or inappropriate behavior
-
Motor dysfunction, presenting as hand tremors and coordination issues
-
In advanced stages, stupor and coma are common
These changes severely impact independence and quality of life, often necessitating full-time caregiving support and palliative care consultation.
What Are Other Complications in End-Stage Liver Failure?
Additional complications include kidney failure in about 20-50% of hospitalized patients and life-threatening bleeding episodes, with 10-20% experiencing fatal hemorrhage through the esophageal varices within six weeks.
Multi-organ system involvement:
-
Kidney dysfunction often requires dialysis support
-
Cardiovascular instability where blood pressure fluctuates with heart rhythm problems
-
Respiratory compromise because of fluid accumulation in the lungs
-
Immune system suppression, which compromises the patient to infection
-
Nutritional deficiency because of problems in protein and vitamin absorption
Regular monitoring of blood pressure and organ function helps medical teams anticipate and manage these multi-organ complications effectively.
What Factors Influence the Liver Failure Death Timeline?
Timeline factors include age, underlying cause, and treatment access, with variations ranging from acute progression within days to chronic advancement over years. Younger patients typically demonstrate better treatment responses and longer survival periods.
Demographic factors significantly impact outcomes, with men experiencing twice the cirrhosis death rates compared to women in similar age groups. Comorbid conditions like diabetes and obesity substantially worsen prognosis across all liver failure types.
Geographic location within the US affects treatment access, with rural patients often experiencing delays in specialized care that can influence survival outcomes.
How Do Age and Overall Health Affect the Timeline?
Advanced age and comorbid conditions significantly shorten survival timelines, with older patients showing reduced treatment tolerance and recovery capacity.
Age-related considerations include:
-
Decreased regenerative capacity
-
Medication tolerance
-
Comorbid obesity
-
Cardiovascular health
-
Immune system function
Demographic statistics show that men face twice the risk of mortality with liver disease than women. The reason is more likely because men tend to consume more alcohol and delay seeking medical care.
How Does the Type of Liver Failure Impact the Timeline?
Acute liver failure progresses suddenly while chronic conditions advance gradually, creating vastly different survival timelines and treatment approaches.
Timeline comparisons:
-
Acute progression with hours to days for life-threatening complications
-
Chronic advancement with years to decades for similar severity levels
-
Acute cases require immediate medical intervention
-
Acute cases may recover completely with timely therapy
Acute liver failure demands immediate emergency room evaluation, while chronic conditions allow time for staged interventions and lifestyle modifications.
How Does Access to Treatment Influence the Timeline?
Treatment access, including transplant availability and palliative care, significantly extends survival and improves quality of life during end-stage disease.
Access disparities in the US:
-
Rural versus urban: Specialized liver centers concentrated in metropolitan areas
-
Insurance coverage: Affects treatment options and transplant eligibility
-
Geographic regions: Organ availability varies significantly across regions
-
Socioeconomic factors: Impact nutrition, housing stability, and medication adherence
Palliative care involvement improves quality of life and often extends survival through better symptom management and psychological support.
How Is Liver Failure Treated and Managed?

Treatment approaches range from medications managing symptoms to liver transplantation, potentially extending life expectancy by years. Early-stage interventions focus on stopping disease progression, while advanced stages require palliative care for comfort and quality of life.
Modern management strategies combine medical treatments, lifestyle modifications, and supportive care to address both the underlying disease and resulting complications. Treatment effectiveness depends heavily on patient compliance and disease stage at diagnosis.
Multidisciplinary care teams including hepatologists, transplant surgeons, and palliative care specialists provide comprehensive management throughout the disease progression.
What Lifestyle Changes Help Manage Liver Failure?
Lifestyle modifications can slow disease progression significantly, with alcohol cessation and weight management representing the most impactful interventions.
Essential lifestyle changes:
-
Alcohol abstinence
-
Weight management
-
Dietary modifications (low-salt diets)
-
Exercise
-
Medication compliance
You can seek nutritional advice from dietary experts for your nutritional needs. This is to manage complications effectively, particularly ascites or hepatic encephalopathy.
What Medications and Procedures Are Used?
Short answer, medical treatments include diuretics for ascites, TIPS procedures for bleeding prevention, and antiviral medications for hepatitis management.
In detail, common interventions include:
-
Diuretic therapy like spironolactone and furosemide to manage excess fluid
-
To reduce portal hypertension and bleeding risk, often beta-blockers are employed
-
Hepatic encephalopathy is often managed with lactulose
-
TIPS (transjugular intrahepatic portosystemic shunt) to reduce pressure
-
Paracentesis for patients with significantly large amounts of ascites (abdominal fluid) particularly when diuretics fail
Side effect monitoring remains crucial, as failing livers process medications differently, requiring dose adjustments and careful observation.
When Is a Liver Transplant Considered?
Liver transplantation consideration occurs when MELD scores reach 15 or higher, with organ allocation prioritizing the sickest patients through objective scoring systems.
Transplant evaluation criteria:
-
MELD scores generally > 15
-
Typical six months abstinence from alcohol (in alcohol-related disease)
-
Psychological evaluation (patient should be stable, good support systems, and good ability to cope)
-
Cardiac clearance
-
Age considerations
Wait times vary dramatically across US regions, with some patients waiting months longer than others based purely on geographic location.
What Role Does Palliative Care Play?
Palliative care improves quality of life throughout the disease course, not just during end-stage phases, while reducing hospitalizations and enhancing symptom management.
Benefits:
-
Symptom management
-
Psychological support
-
Goals of care
-
Care coordination
-
Advanced directives
Research shows that early palliative care significantly reduces hospital deaths and improves patient satisfaction scores.
Quick Summary Box:
-
Timeline Range: Days (acute) to years (chronic)
-
Survival Rates: 75% acute cases, 50% two-year chronic
-
Key Symptoms: Jaundice, confusion, abdominal swelling
-
Treatment Options: Lifestyle changes, medications, transplant
-
Early Detection: Critical for better outcomes and extended survival
Related Resources
What is a Liver Abscess? Symptoms, Causes, Diagnosis, and Treatment
What is an Echogenic Liver? Understanding Ultrasound Findings
References
Agrawal, S., & Khazaeni, B. (2023, June 9). Acetaminophen toxicity. National Library of Medicine; StatPearls Publishing. https://www.ncbi.nlm.nih.gov/books/NBK441917/
Amesur, N. B., & Novelli, P. (2023, July 24). Transjugular Intrahepatic Portosystemic Shunt. PubMed; StatPearls Publishing. https://www.ncbi.nlm.nih.gov/books/NBK513268/
Aponte, E. M., & O’Rourke, M. C. (2019). Paracentesis. Nih.gov; StatPearls Publishing. https://www.ncbi.nlm.nih.gov/books/NBK435998/
Appenrodt, B., & Lammert, F. (2018). Renal Failure in Patients with Liver Cirrhosis: Novel Classifications, Biomarkers, Treatment. Visceral Medicine, 34(4), 246–253. https://doi.org/10.1159/000492587
Chronic liver disease death rates worldwide by gender 2019| Statista. (2019). Statista. https://www.statista.com/statistics/1482510/death-rate-from-liver-cirrhosis-and-other-chronic-liver-diseases-worldwide-by-gender/
Harrison, P. M. (2015). Management of patients with decompensated cirrhosis. Clinical Medicine, 15(2), 201–203. https://doi.org/10.7861/clinmedicine.15-2-201
Hashim, I. A. (2024, January 1). Chapter 4 - Liver function (I. A. Hashim, Ed.). ScienceDirect; Elsevier. https://www.sciencedirect.com/science/article/pii/B9780128229491000085
Kardashian, A., Serper, M., Terrault, N., & Nephew, L. D. (2022). Health disparities in chronic liver disease. Hepatology, 77(4). https://doi.org/10.1002/hep.32743
L.M. Martínez-Martínez, G. Rosales-Sotomayor, E.A. Jasso-Baltazar, J.A. Torres-Díaz, D. Aguirre-Villarreal, de, H.-D., V.M. Páez-Zayas, A. Sánchez-Cedillo, S.E. Martínez-Vázquez, H.N. Tadeo-Espinoza, J.P. Guerrero-Cabrera, M. García-Alanis, & I. García-Juárez. (2024). Acute liver failure: Management update and prognosis. Revista de Gastroenterología de México (English Edition), 89(3), 404–417. https://doi.org/10.1016/j.rgmxen.2024.05.002
Ladin, K., & Hanto, D. W. (2017). Are geographic differences in transplantation inherently wrong? Current Opinion in Organ Transplantation, 22(2), 174–178. https://doi.org/10.1097/mot.0000000000000400
Lazarus, J. V., Mark, H. E., Villota-Rivas, M., Palayew, A., Carrieri, P., Colombo, M., Ekstedt, M., Esmat, G., George, J., Marchesini, G., Novak, K., Ocama, P., Ratziu, V., Razavi, H., Romero-Gómez, M., Silva, M., Spearman, C. W., Tacke, F., Tsochatzis, E. A., & Yilmaz, Y. (2022). The global NAFLD policy review and preparedness index: Are countries ready to address this silent public health challenge? Journal of Hepatology, 76(4), 771–780. https://doi.org/10.1016/j.jhep.2021.10.025
Liu, X., Chang, Y.-C., & Hu, W.-Y. (2024). The Effectiveness of Palliative Care Interventions in Long-Term Care Facilities: A Systematic Review. Journal of Personalized Medicine, 14(7), 700. https://doi.org/10.3390/jpm14070700
Mahmud, N. (2020). Selection for Liver Transplantation: Indications and Evaluation. Current Hepatology Reports, 19(3), 203–212. https://doi.org/10.1007/s11901-020-00527-9
Mandiga, P., Foris, L. A., Kassim, G., & Bollu, P. C. (2025, January 20). Hepatic Encephalopathy. National Library of Medicine; StatPearls Publishing. https://www.ncbi.nlm.nih.gov/books/NBK430869/
Meseeha, M., & Attia, M. (2023, August 7). Esophageal Varices. Nih.gov; StatPearls Publishing. https://www.ncbi.nlm.nih.gov/books/NBK448078/
Monnig, M. A., Padovano, H. T., & Monti, P. M. (2024). Alcohol-associated liver disease and behavioral and medical cofactors: unmet needs and opportunities. Frontiers in Public Health, 12. https://doi.org/10.3389/fpubh.2024.1322460
Patra, J., Buckley, C., Kerr, W. C., Brennan, A., Purshouse, R. C., & Rehm, J. (2021). Impact of body mass and alcohol consumption on all‐cause and liver mortality in 240 000 adults in the United States. Drug and Alcohol Review. https://doi.org/10.1111/dar.13265
Potosek, J., Curry, M., Buss, M., & Chittenden, E. (2014). Integration of Palliative Care in End-Stage Liver Disease and Liver Transplantation. Journal of Palliative Medicine, 17(11), 1271–1277. https://doi.org/10.1089/jpm.2013.0167
Reuben, A., Tillman, H., Fontana, R. J., Davern, T., McGuire, B., Stravitz, R. T., Durkalski, V., Larson, A. M., Liou, I., Fix, O., Schilsky, M., McCashland, T., Hay, J. E., Murray, N., Shaikh, O. S., Ganger, D., Zaman, A., Han, S. B., Chung, R. T., & Smith, A. (2016). Outcomes in Adults With Acute Liver Failure Between 1998 and 2013. Annals of Internal Medicine, 164(11), 724. https://doi.org/10.7326/m15-2211
Shah, N. J., Royer, A., & John, S. (2023). Acute liver failure. PubMed; StatPearls Publishing. https://www.ncbi.nlm.nih.gov/books/NBK482374/
Singal, A. K., & Kamath, P. S. (2013). Model for End-stage Liver Disease. Journal of Clinical and Experimental Hepatology, 3(1), 50–60. https://doi.org/10.1016/j.jceh.2012.11.002
Tapper, E. B., & Parikh, N. D. (2018). Mortality due to cirrhosis and liver cancer in the United States, 1999-2016: observational study. BMJ, 362, k2817. https://doi.org/10.1136/bmj.k2817
UpToDate. (n.d.). Www.uptodate.com. https://www.uptodate.com/contents/image?imageKey=GAST%2F78401
Vignesh Krishnan Nagesh, Varughese, V. J., Basta, M., Martinez, E., Shruthi Badam, Lokaesh Subramani Shobana, Mohamed, A., Alin J, Weissman, S., & Atoot, A. (2025). Trends and Disparities in Liver Transplantation in the United States: A Nationwide Analysis of Demographic, Clinical, and Socioeconomic Factors (2016–2021). Medical Sciences, 13(2), 66–66. https://doi.org/10.3390/medsci13020066

Jaclyn P. Leyson-Azuela, RMT, MD, MPH, is a licensed General Practitioner and Public Health Expert. She currently serves as a physician in private practice, combining clinical care with her passion for preventive health and community wellness.




