Fungal UTI: Symptoms, Causes, and Treatment You Should Know
 Written By
Blen Shumiye, MD
Written By
Blen Shumiye, MD
When you hear “UTI,” you probably think of a bacterial infection. But if you’ve dealt with recurring urinary issues, use a catheter, or manage conditions like diabetes or a weakened immune system, it’s worth being aware of another type: fungal urinary tract infections. They’re less common and are trickier to treat.
In this article, you’ll learn what a fungal UTI is, how to recognize the signs, what causes it, and how it’s treated so you can feel more informed, empowered, and proactive about your health.
What is a fungal UTI?
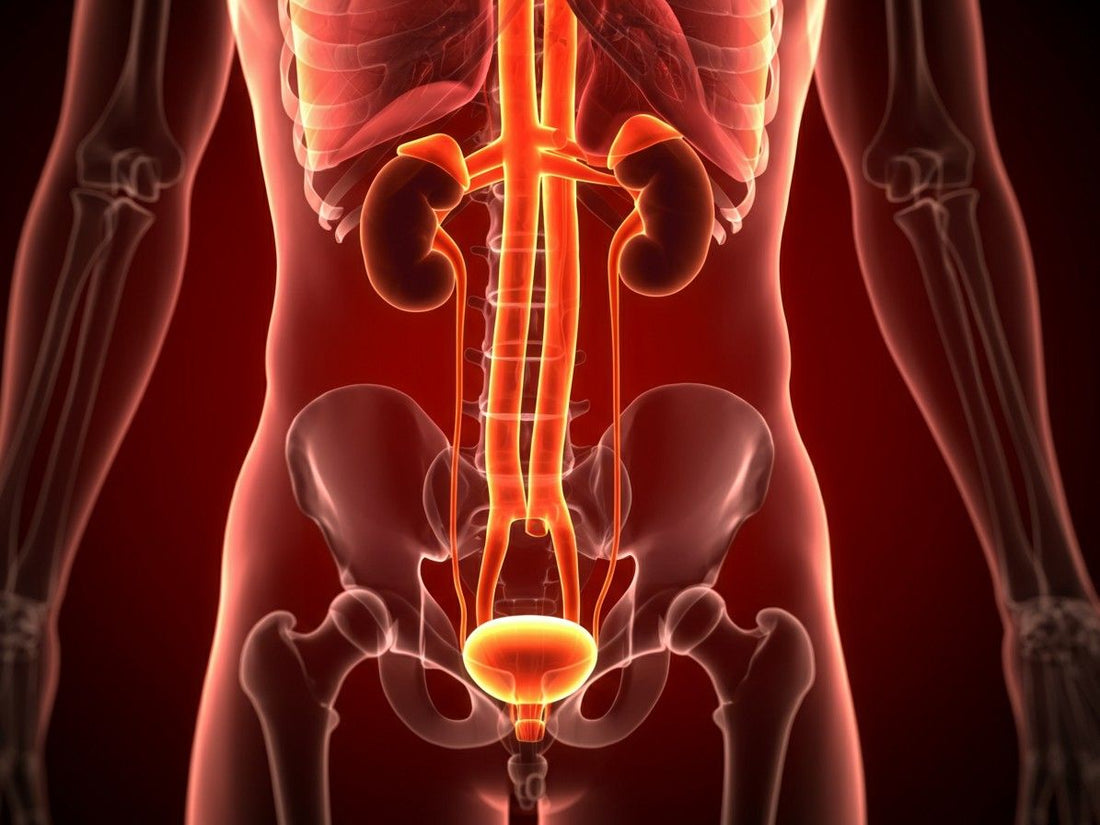
A fungal urinary tract infection (UTI) occurs when fungi—most often Candida species—infect the urinary system. Bacterial infections are far more common, fungal UTIs can develop under certain conditions, particularly when the body’s natural defenses are compromised.
They tend to affect individuals with risk factors such as catheter use, diabetes, recent antibiotic use, or a weakened immune system. These infections can involve the bladder (cystitis), kidneys (pyelonephritis), or urethra, and in some cases, may spread from other areas of the body through the bloodstream.
What causes a fungal UTI?
Here are common causes and contributing factors:
-
Catheter use: Prolonged catheterization can give fungi a direct pathway into the bladder. Biofilms—protective layers that form on catheter surfaces—can harbor fungal cells and resist treatment.
-
Recent antibiotic use: Antibiotics may wipe out helpful bacteria in the urinary and digestive tracts, allowing Candida to multiply unchecked.
-
Diabetes: Elevated blood sugar levels not only feed fungal growth but also impair immune response.
-
Immune suppression: Conditions like HIV/AIDS, cancer, or the use of immunosuppressive medications make it harder for the body to control fungal overgrowth.
-
Recent urologic procedures: Surgeries or devices such as stents or nephrostomy tubes can disrupt the urinary tract, making it easier for fungi to establish infection.
-
Systemic fungal infections: In some cases, fungi can spread through the bloodstream from another infected site—such as the gut or lungs—and reach the kidneys.
What are the symptoms of a fungal UTI?

Most fungal UTIs don’t cause obvious symptoms, especially in the early stages. However, when they do, symptoms can vary based on which part of the urinary tract is affected.
Common symptoms
-
Burning or pain while urinating (dysuria)
-
Urgency to urinate
-
Blood in the urine (hematuria)
-
Cloudy or foul-smelling urine (urine color can signal an active infection or imbalance.)
-
Pain or pressure in the lower abdomen
-
Fever or chills
-
Fatigue or general malaise
It’s important to note that vaginal yeast infections are different from fungal UTIs, though they may occur together. Vaginal itching, thick white discharge, and external irritation are signs of a vaginal yeast infection, not necessarily a fungal UTI—but they may co-exist, especially in people with systemic fungal overgrowth.
Red flags to watch for
If the infection spreads to the kidneys or becomes systemic (enters the bloodstream), symptoms can become more serious:
-
High fever
-
Chills
-
Nausea and vomiting
-
Severe back pain
These are red flags and warrant immediate medical attention. Delayed diagnosis and treatment can lead to complications such as kidney damage or systemic candidiasis, which is a medical emergency.
Possible complications
Here are some rare but serious complications that can occur with fungal UTIs, especially in high-risk individuals:
-
Fungus balls: Clumps of fungal cells that can block the ureters or bladder.
-
Emphysematous cystitis: A rare complication in people with diabetes where gas forms in the bladder wall.
-
Kidney abscesses or papillary necrosis: May cause flank pain, fever, or worsening kidney function.
How is a fungal UTI diagnosed?

Because fungal UTIs present similarly to bacterial UTIs, proper diagnosis is essential before beginning treatment.
Diagnostic Steps Include:
-
Urine Culture: A urine culture is the gold standard way to detect fungi like Candida. However, a positive result doesn’t always mean you have an active infection—it could also indicate colonization (fungi present but not causing illness).
-
Microscopic Examination: Lab technicians may spot yeast cells directly under a microscope.
-
Urinalysis: This tests for signs of infection like white blood cells, but it won’t confirm the cause. It’s typically used in combination with culture tests.
-
Blood Tests (if needed): In severe cases or if a systemic infection is suspected, blood tests may be done to check for fungal infection beyond the urinary tract.
-
Imaging (ultrasound or CT scan): Helps find fungus balls, kidney abscesses, or bladder wall inflammation.
It’s crucial that a healthcare professional interprets these results in context. Sometimes, Candida in the urine may not indicate an infection at all—especially in asymptomatic individuals with catheters.
When should you treat a fungal UTI?
Unlike bacterial UTIs, fungal UTIs aren’t always treated right away. In fact, if you don’t have symptoms and aren’t at high risk, treatment may not be necessary.
You may need treatment if:
-
You have symptoms (burning, frequency, pain)
-
You’re neutropenic (low white blood cell count)
-
You’re undergoing urologic surgery soon
-
You’ve had a kidney transplant
What are the treatment options?

Your treatment depends on the severity of your infection, the fungal species, and whether you have any medical devices like catheters in place.
Antifungal medications
-
Fluconazole is often the first choice for treating Candida albicans. It's taken orally at 200–400 mg daily for about 14 days.
-
Amphotericin B is used for infections resistant to fluconazole and is given intravenously. It may be combined with flucytosine in more severe cases.
-
Flucytosine is taken by mouth and dosed based on kidney function. It’s usually paired with another antifungal to reduce the risk of resistance.
Removing medical devices
-
If possible, your catheter or stent should be removed to prevent recurrence.
Monitoring and follow-up
-
Follow-up urine cultures may be done to confirm that the infection is gone.
Can fungal UTIs come back?
Yes. Even after successful treatment, fungal UTIs can return—especially if the underlying risk factors like catheter use or high blood sugar aren't addressed.
To lower your chances of recurrence:
-
Limit use of catheters
-
Treat any fungal overgrowth promptly
How can you prevent a fungal UTI?
Prevention is especially important if you have any of the risk factors. Smart prevention tips:
-
Only use urinary catheters when absolutely necessary
-
Remove catheters as soon as possible
-
Take antibiotics only when prescribed
-
Manage your blood sugar levels if you have diabetes
-
Stay hydrated to flush out your urinary tract
-
Monitor for symptoms if you’re immunocompromised
-
Be aware of foods to avoid with UTI
-
Understand urine pH and what abnormal urine pH could mean.
What should you do if you think you have a fungal UTI?
If you're experiencing any symptoms of a UTI and have risk factors like diabetes, catheter use, or a weakened immune system, see a healthcare provider. They may order urine tests, imaging, or bloodwork to determine the best next steps.
Do not self-diagnose or self-treat fungal infections, as improper treatment can lead to complications or resistance.
Final Takeaway
Fungal UTIs may be uncommon, but for those with diabetes, catheters, or weakened immunity, they can be an early sign that something’s out of balance. While they may not always cause symptoms, their presence is a signal worth paying attention to—not a cause for panic.
The encouraging news is that they’re manageable. With proper diagnosis, timely treatment, and a few preventive habits—like limiting catheter use, managing blood sugar, and staying hydrated—you can lower your risk and support your urinary health.
Awareness is the first step. With consistent care and small, steady changes, you can protect your body, feel more in control, and reduce the chances of future infections.
Stay ahead of complications and use Ribbon Checkup to track your urinary health.
Related resources
References
Imam, T. H. (2024, January 5). Fungal Urinary Tract Infections. MSD Manual Professional Edition; MSD Manuals. https://www.msdmanuals.com/professional/genitourinary-disorders/urinary-tract-infections-utis/fungal-urinary-tract-infections#Treatment_v1053095
Kauffman, C. A. (2013). Diagnosis and Management of Fungal Urinary Tract Infection. Infectious Disease Clinics of North America, 28(1), 61–74. https://doi.org/10.1016/j.idc.2013.09.004
Kauffman, C. A., Fisher, J. F., Sobel, J. D., & Newman, C. A. (2011). Candida Urinary Tract Infections—Diagnosis. Clinical Infectious Diseases, 52(suppl_6), S452–S456. https://doi.org/10.1093/cid/cir111
S Krcmery. (1999). Fungal urinary tract infections in patients at risk. International Journal of Antimicrobial Agents, 11(3-4), 289–291. https://doi.org/10.1016/s0924-8579(99)00032-1
CDC. (2025, June 27). Catheter-associated Urinary Tract Infection (CAUTI) Basics. Urinary Tract Infection. https://www.cdc.gov/uti/about/cauti-basics.html

Dr. Blen is a seasoned medical writer and General Practitioner with over five years of clinical experience. She blends deep medical expertise with a gift for clear, compassionate communication to create evidence-based content that informs and empowers. Her work spans clinical research, patient education, and health journalism, establishing her as a trusted voice in both professional and public health spheres.


