Bladder Infection vs UTI Symptoms: A Comprehensive Clinical Comparison
 Written By
Jaclyn P. Leyson-Azuela, RMT, MD, MPH
Written By
Jaclyn P. Leyson-Azuela, RMT, MD, MPH
When you experience painful urination, urgency, or discomfort in the lower abdomen, one common question that arises include: “what are bladder infection vs UTI symptoms” This is often a cause of concern because often they are interchanged even in causal medical discussions. But understanding the differences, and the relationship, between bladder infections and urinary tract infections (UTIs) is essential for making an accurate diagnosis, receiving appropriate treatment, and effective preventive strategies.
This article will guide you on the clinical, diagnostic, and other distinctive characteristics of bladder infection and UTIs. You will learn evidence-based information so you can make informed choices about your health and be proactive about it.
Key Insights:
-
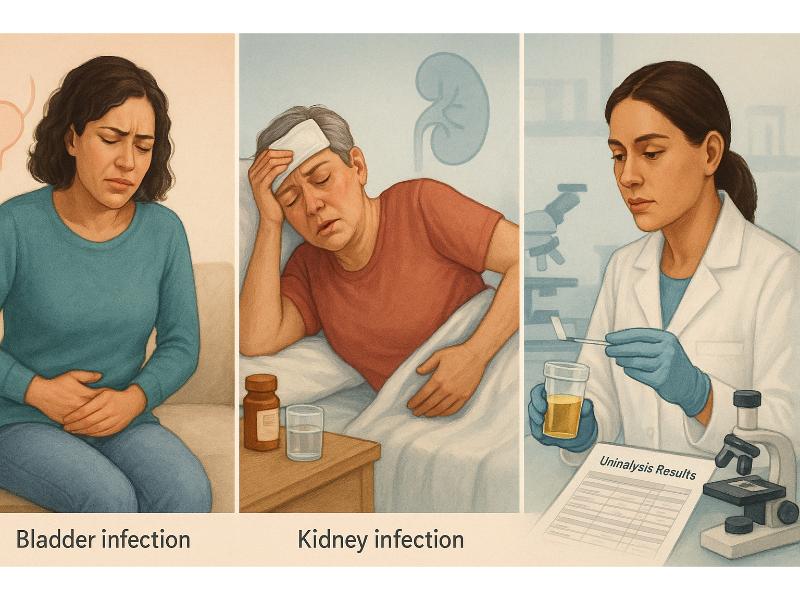
Bladder infections are a type of UTI, but UTIs can also affect the kidneys, ureter, and urethra
-
Symptoms vary by location; bladder infection often causes localized discomfort, while kidney infections may cause fever, nausea, or back pain
-
E. coli is the leading cause of most UTIs
-
Women are more susceptible to developing UTIs than men due to their unique anatomical factors
-
Diagnosis involves urine tests but may involve blood work as well
-
Antibiotics are the primary mode of treatment although home remedies may offer symptom relief but not cure
-
Seek medical health immediately for severe symptoms like high fever, vomiting, back pain, or confusion
What is the Difference Between a Bladder Infection and a UTI?
To start with, it’s important to recognize that a bladder infection is one of the many types of UTI—a basic concept you need to understand. To be more precise, a bladder infection is also known as cystitis, which is categorized as a lower urinary tract infection. So it goes without saying that the term UTI is a broader umbrella, encompassing infections of the entire urinary tract, including:
-
Lower UTI–affects the urethra and bladder (e.g., cystitis)
-
Upper UTI–affects the ureters and kidneys (e.g., pyelonephritis)
So, while all bladder infections are UTIs, not all UTIs are limited to the bladder.
Why Understanding the Difference Matters?

From a clinical perspective, recognizing the difference between a bladder infection and an upper UTI is crucial. An untreated bladder infection may progress into a more serious upper UTI. It could potentially lead to kidney damage, systemic infection (sepsis), or other complications. Knowing the anatomy, symptom profiles, and risk factors allows both patients and clinicians for early and appropriate intervention.
Symptoms of a Bladder Infection (Cystitis)
Bladder infections are typically localized and non-systemic. Most symptoms are confined to the lower urinary tract. Key signs include the following:
-
Dysuria–burning or tingling sensation during urination; you are 7.8 times more likely to experience this symptom, which makes it a common symptom for many patients
-
Increased urinary frequency–the need to urinate more often than usual; in some cases it occurs every 30-60 minutes
-
Urgency–this is the sensation of a compelling, often uncontrollable urge to urinate
-
Suprapubic pain–discomfort or tenderness just above the pubic bone
-
Change in urine appearance or smell–cloudy, dark, or foul-smelling urine
-
Hematuria–presence of blood in the urine; there are times when you can see it visibly in the urine but in many cases it is only visible under the microscope
-
Sensation of incomplete bladder emptying–a persistent feeling that the bladder has not been emptied
What is Typically Absent?
Typical symptoms that are absent include:
-
Fever is often rare or low-grade
-
Systemic symptoms like chills or vomiting are uncommon
-
Flank pain (pain in the back or side) is not a primary symptom
Symptoms of an Upper UTI — Pyelonephritis
Pyelonephritis is a more serious infection that affects the kidneys, which often causes systemic illness.
-
High fever—often a temperature of ≥38°C (100.4°F); most reliable indicator of upper UTI
-
Flank pain—pain and tenderness on either or both sides; it is often near the back and under the ribs
-
Costovertebral angle tenderness—sensitivity when pressing the back near where the kidneys are located
-
Nausea and vomiting—this is one of the most common symptoms
-
Chills and rigors—involuntary shaking due to high fever
-
Fatigue or malaise—often more pronounced due to systemic inflammation
Some symptoms are variable, even the most common symptoms like dysuria and urgency are absent in about 20% of pyelonephritis cases. The lack of urinary symptoms does not, however, rule out an upper UTI.
Research shows that UTIs can have incomplete presentations, where pain and lower urinary tract symptoms are absent in 17.8% and 52.9% of cases, respectively.
Clinical Diagnosis—How Are UTIs and Bladder Infections Diagnosed?

Diagnosis involves a combination of clinical presentation and laboratory testing.
Urinalysis
This is a standard test to detect the following:
-
Pyuria—presence of white blood cells in the urine; often seen in about 50-90% of cases
-
Bacteriuria—presence of bacteria
-
Nitrites and leukocyte esterase—this is suggestive of bacterial infection particularly in gram-negative organisms
Urine Culture
The test is used to:
-
Identify the specific pathogen
-
Guides targeted antibiotic therapy
Blood Tests
This is used especially for suspected pyelonephritis:
-
Elevated C-reactive protein (CRP) or procalcitonin levels
-
These markers suggest systemic inflammation
-
It can help distinguish between the upper and lower UTI
How Do UTIs Develop?
The ascending infection model is often the common explanation why UTIs develop, including pyelonephritis. This model explains that most UTIs start in the urethra and ascend to the bladder. The UTI-induced bladder inflammation leads to afferent neuron sensitization, which causes the common symptoms like frequency, pelvic pain, and urgency. If untreated or if the immune system is compromised, the bacteria can move further to the ureters and finally, the kidneys.
Bladder Inflammatory Response
-
Uropathogenic Escherichia coli (E. coli) is responsible for about 85% of cases
-
These bacteria use fimbriae and adhesins that will stick to the bladder wall
-
The infection triggers cytokine release (which are inflammatory markers released by the body in response to the infection in an attempt to control it); it will lead to:
-
Nerve sensitization
-
Urgency and frequency
-
Pain and inflammation
Overlap with Other Conditions—Overactive Bladder vs UTI
Many symptoms of a bladder infection can overlap or even mimic with other conditions, such as overactive bladder (OAB). The symptoms could include:
-
Urgency
-
Frequency
-
Urge incontinence
The similarity of symptoms can lead to misdiagnosis. So advanced urine culture techniques, including enhanced quantitative urine culture (EQUC). The test can detect low-colony count or intracellular pathogens, which can be missed by other standard methods.
Treatment Guidelines for Bladder Infection vs UTI
Bladder Infection (Uncomplicated Cystitis)
-
Antibiotics are typically prescribed for 3-7 days, such as nitrofurantoin and trimethoprim-sulfamethoxazole
-
Oral therapy is generally efficient and effective
-
Outpatient management is normal for these cases
Upper UTI (Pyelonephritis)
-
Antibiotics are still prescribed but the duration is prolonged for 10-14 days
-
Often begins with IV antibiotics, which means you need to get hospitalized for a few days to get the appropriate treatment; this is often for severe cases that require hospitalization
-
The IV antibiotics will then be switched to oral regimen once your symptoms improve
What Are The Risks of Untreated UTIs?
Leaving UTI untreated can lead to serious health consequences, as the infection could potentially spread and affect other parts of the body. Appropriate treatment should be initiated to prevent these complications.
-
Kidney infection (pyelonephritis). The most significant risk for untreated UTI infection is if it spreads from the bladder to one or both kidneys, which could potentially lead to acute kidney injury or even permanent damage like scarring.
-
Recurrent UTIs. Untreated or improperly treated UTI can lead to a cycle of recurrent infections, which make it harder to manage over time.
-
Sepsis. This complication is rare but may happen in severe cases. It is a life-threatening condition that is caused by the body’s overwhelming response to an infection. Multiple organs may be affected or get shut down. The risk is higher for patients who have weakened immune systems.
-
Pregnancy complications. For pregnant women, untreated UTIs can increase the risk of having premature birth or low birth weight for babies.
-
Urethral stricture. In men, recurrent and untreated UTIs could lead to narrowing of the urethra, which is called stricture formation.
When should you see a doctor for recurring UTIs?
If you are experiencing frequent UTIs, it is important that you consult your primary care so you can identify the underlying causes and plan for long-term management. Recurring UTIs are defined as having more than 2 acute UTIs in six months or a minimum of 3 in 12 months. Generally, women are more susceptible for recurrent UTIs, which occurs in about 20-30% of women.
You should see a doctor if you have the following:
-
Frequent episodes even after treatment
-
Persistent symptoms despite completing the antibiotic treatment
-
Underlying conditions:
-
Kidney stones
-
Urethral strictures or narrowing
-
Immunocompromised state
-
Postmenopausal
Women in this group with recurrent UTI would benefit from management like vaginal estrogen therapy.
-
Frequent episodes in men
UTIs are less common in men so it often requires further investigation to rule out prostate issues or any other underlying cause
Red Flags—When a Bladder Infection Becomes Serious?

Warning signs for UTI
Watch for these signs, which indicate possible progression to upper UTI:
-
Fever more than 38.5°C (101.3°F)
-
New or worsening flank pain
-
Nausea or vomiting
-
Chills, confusion, or rapid breathing
-
Signs of systemic toxicity
Do Special Populations Have Atypical Presentations?
Yes, special populations often present atypically or unusually.
What are these special populations?
Elderly patients:
-
May present with confusion, falls, or agitation
-
Classic symptoms may be absent
-
Higher risk of complications, including urosepsis
Immunocompromised individuals:
-
Includes diabetic and cancer patients and transplant recipients
-
Also includes individuals with underlying medical conditions that require immunosuppressants
-
These patients often have blunted or weakened immune response
-
Early intervention and close monitoring are required
Prevention Strategies for Recurrent Bladder Infections and UTIs

Whether you are dealing with recurrent UTI or simply want to reduce your risk, there are simple preventive strategies you can practice. It includes:
-
Hydration–depending on your activity level, increase your fluid intake accordingly; diluting your urine can potentially flush out bacteria
-
Complete bladder emptying–avoid holding your urine for prolonged periods
-
Hygiene–for women, wiping from front to back often helps to prevent infection. Also, use gentle soaps on your genital area
-
Post-coital urination
-
Avoiding irritants–bubble baths, douches, and perfumed products often irritate the urethra, which may cause disruption of the normal flora (good organisms in the genital area)
Conclusion
Bladder infections are a type of UTI, which are common conditions especially among women. It causes symptoms that are localized to the lower UTI but it may involve the upper tract, which poses bigger risks.
By understanding the symptom patterns, diagnostic strategies, and treatment differences, patients and healthcare providers can work together to manage urinary tract infections effectively.
If you’re experiencing persistent or severe urinary symptoms, seek medical attention promptly. Early intervention not only relieves symptoms faster but also reduces the risk of serious complications.
Quick Summary Box
-
A bladder infection is a subtype of UTI affecting the bladder specifically.
-
Kidney infections are more serious and present with fever, back pain, and nausea.
-
E. coli is the primary cause; women are most at risk.
-
Urine tests confirm diagnosis; antibiotics are essential for treatment.
-
Seek urgent care for severe symptoms to avoid complications like kidney damage or sepsis.
Related Resources
UTI Symptoms Men: What It Is, Causes, Diagnosis, Treatment, and Prevention
UTI Tests: The Essential Guide to Understanding and Managing Your Health
References
Aggarwal, N., & Leslie, S. W. (2025). Recurrent urinary tract infections. PubMed; StatPearls Publishing. https://www.ncbi.nlm.nih.gov/books/NBK557479/
Christmas, M. M., Iyer, S., Daisy, C., Maristany, S., Letko, J., & Hickey, M. (2023). Menopause hormone therapy and urinary symptoms: a systematic review. Menopause (New York, N.Y.), 30(6), 672–685. https://doi.org/10.1097/GME.0000000000002187
Fauziansyah, A., Fahrul Arifin, M., Ubaidillah Faqih, Moh., Karyo, & Wahdini, R. (2025). Edukasi Infeksi Saluran Kemih Pada Ibu PKK Di Desa Temayang, Kerek, Tuban. Service Quality (Jurnal Pengabdian Masyarakat), 2(1), 115–122. https://doi.org/10.33377/sqj.v2i1.255
Herness, J., Buttolph, A., & Hammer, N. C. (2020). Acute pyelonephritis in adults: Rapid evidence review. American Family Physician, 102(3), 173–180. https://www.aafp.org/pubs/afp/issues/2020/0801/p173.html
Hertz, M. A., Skjøt-Arkil, H., Heltborg, A., Lorentzen, M. H., Cartuliares, M. B., Rosenvinge, F. S., Nielsen, S. L., Mogensen, C. B., & Johansen, I. S. (2024). Clinical characteristics, factors associated with urinary tract infection and outcome in acutely admitted patients with infection; an exploratory cross-sectional cohort study. Heliyon, 10(12), e32815. https://doi.org/10.1016/j.heliyon.2024.e32815
Hsu, C.-K., Wu, S.-Y., Yang, S.-D., & Chang, S.-J. (2022). Emphysematous pyelonephritis: classification, management, and prognosis. Tzu Chi Medical Journal, 34(3), 297. https://doi.org/10.4103/tcmj.tcmj_257_21
Ke, Q.-S., Lee, C.-L., & Kuo, H.-C. (2020). Recurrent urinary tract infection in women and overactive bladder – Is there a relationship? Tzu-Chi Medical Journal, 33(1), 13–21. https://doi.org/10.4103/tcmj.tcmj_38_20
Khan, Z., Healey, G. D., Paravati, R., Berry, N., Rees, E., Margarit, L., Deyarina González, Emery, S., & R. Steven Conlan. (2021). Chronic Urinary Infection in Overactive Bladder Syndrome: A Prospective, Blinded Case Control Study. Frontiers in Cellular and Infection Microbiology, 11. https://doi.org/10.3389/fcimb.2021.752275
Kobayashi, K., Yamashita, K., Mizuno, S., Kubo, K., Komiya, N., & Otsu, S. (2022). External validation of a clinical prediction rule on the need for radiologic imaging to identify urological disorders in adult patients with febrile urinary tract infections. Singapore Medical Journal, 63(3), 167–169. https://doi.org/10.11622/smedj.2022047
Montalbetti, N., Dalghi, M. G., Bastacky, S. I., Clayton, D. R., Ruiz, W. G., Apodaca, G., & Carattino, M. D. (2022). Bladder infection with uropathogenic Escherichia coli increases the excitability of afferent neurons. American Journal of Physiology-Renal Physiology, 322(1), F1–F13. https://doi.org/10.1152/ajprenal.00167.2021
Piccoli, G. B., Consiglio, V., Deagostini, M. C., Serra, M., Marilisa Biolcati, Ragni, F., Biglino, A., Pascale, A. D., Frascisco, M. F., Veltri, A., & Porpiglia, F. (2011). The clinical and imaging presentation of acute “non complicated” pyelonephritis: A new profile for an ancient disease. BMC Nephrology, 12(1). https://doi.org/10.1186/1471-2369-12-68
Porat, A., & Kesler, S. (2023, August 17). Urosepsis. PubMed; StatPearls Publishing. https://www.ncbi.nlm.nih.gov/books/NBK482344/
Pyuria - an overview | ScienceDirect Topics. (n.d.). Www.sciencedirect.com. https://www.sciencedirect.com/topics/pharmacology-toxicology-and-pharmaceutical-science/pyuria
Sangeeta S. H, Sahana M, & Waheeda Banu. (2024). An insight into Pittaja Mutrakrichra w.s.r. to Lower Urinary Tract Infection with mechanism, risk factors & prevention. Journal of Ayurveda and Integrated Medical Sciences, 9(9), 200–205. https://doi.org/10.21760/jaims.9.9.32
Silva, M. M., Costa, A. B., & Baptista, C. E. (2023). A Rare Case of Recurrent Cystitis in a Primary Care Setting. Cureus. https://doi.org/10.7759/cureus.48914

Jaclyn P. Leyson-Azuela, RMT, MD, MPH, is a licensed General Practitioner and Public Health Expert. She currently serves as a physician in private practice, combining clinical care with her passion for preventive health and community wellness.


