Understanding Creatinine Levels: A Comprehensive Guide
 Written By
Analytics Delante
Written By
Analytics Delante
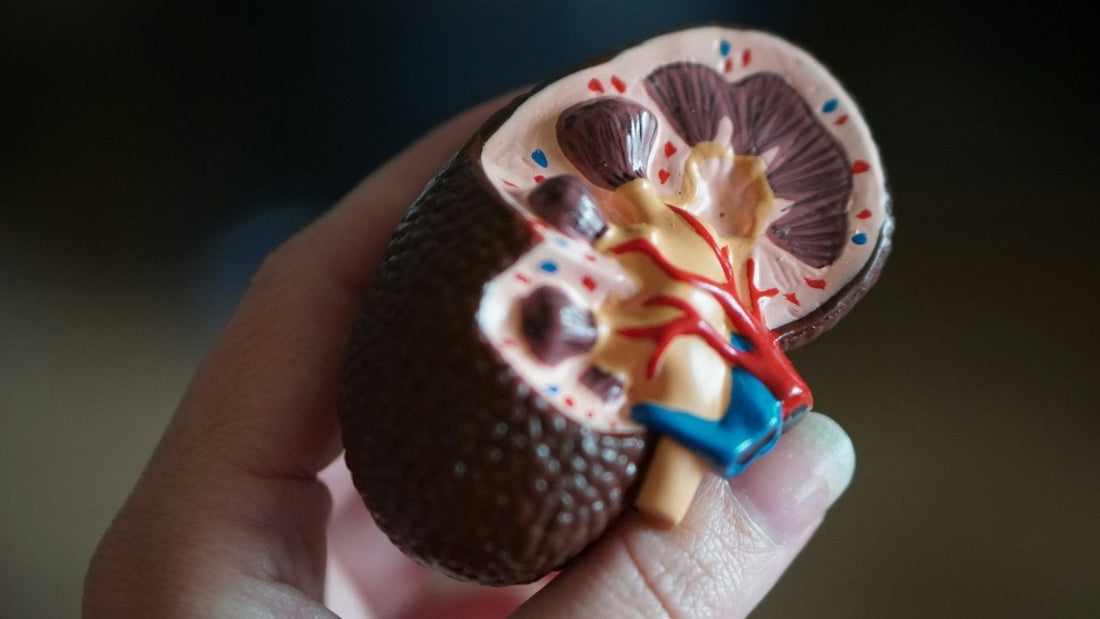
Creatinine is a waste product generated from the natural breakdown of creatine in muscles. Since muscle tissue continuously metabolizes creatine, creatinine is produced at a relatively steady rate. It enters the bloodstream and is filtered out by the kidneys before being excreted in urine. Because of this process, creatinine levels in both blood and urine provide valuable insights into kidney function.
The Creatinine Test: Purpose and Significance
The creatinine test measures creatinine concentration in bodily fluids and is an essential tool for assessing kidney health. Healthcare providers use creatinine tests to:
- Evaluate Kidney Function: Elevated creatinine levels can indicate impaired kidney function, prompting further examination.
- Diagnose Kidney Disease: Persistent high creatinine levels may suggest conditions such as chronic kidney disease (CKD), acute kidney injury (AKI), or urinary tract obstruction.
- Monitor Treatment Effectiveness: Individuals with kidney-related disorders require regular creatinine tests to track treatment progress and disease progression.
- Detect Medication Side Effects: Certain drugs can impact kidney function, and monitoring creatinine levels helps identify potential nephrotoxicity.
See Related: Stages of Chronic Kidney Disease. Know the CKD Symptoms
Types of Creatinine Tests
Several methods assess creatinine levels, each serving different diagnostic purposes:
- Blood Creatinine Test: A blood sample is analyzed to measure creatinine concentration. Elevated levels may suggest kidney dysfunction or disease.
- Urine Creatinine Test: This test complements blood measurements and can involve either a single void sample or a 24-hour urine collection to evaluate kidney performance.
What Does a High Creatinine Level Mean?
Creatinine levels vary depending on factors such as age, sex, muscle mass, and hydration status. Normal serum creatinine reference ranges are:
- Adult males: 0.7 to 1.2 mg/dL
- Adult females: 0.5 to 1.0 mg/dL
Deviations from these ranges may indicate underlying renal dysfunction or other conditions affecting creatinine metabolism.
Factors Influencing Creatinine Levels

Several factors can impact creatinine levels, including:
- Chronic Kidney Disease (CKD): Progressive renal dysfunction leads to impaired creatinine clearance, resulting in elevated levels.
- Urinary Tract Obstruction: Conditions like kidney stones or ureteral strictures can prevent normal creatinine excretion.
- Protein-Rich Diet: High protein intake may temporarily increase creatinine levels due to enhanced muscle metabolism.
- Intense Exercise: Strenuous activity can cause transient creatinine elevation due to increased muscle breakdown.
- Medications: Some drugs, including NSAIDs and certain antibiotics, can affect kidney function and alter creatinine levels.
- Low Muscle Mass: Conditions like malnutrition or neuromuscular disorders can lead to lower serum creatinine levels.
Normal Creatinine Levels During Pregnancy
Pregnancy induces physiological changes in kidney function, including increased renal blood flow and glomerular filtration rate (GFR). As a result, serum creatinine levels decrease compared to non-pregnant individuals. Monitoring kidney function during pregnancy is crucial, as deviations from normal levels may indicate conditions like preeclampsia or gestational hypertension.
Understanding Test Results
Beyond creatinine levels, additional parameters provide a comprehensive assessment of kidney health:
- Glomerular Filtration Rate (GFR): A calculated value based on serum creatinine, age, sex, and race. A GFR below 60 mL/min/1.73m² suggests reduced kidney function.
- Creatinine Clearance: Measured from a 24-hour urine collection, this test evaluates how efficiently the kidneys remove creatinine from the blood.
- Urine Albumin to Creatinine Ratio (UACR): Helps detect kidney damage by measuring urinary albumin levels relative to creatinine concentration.
Next Steps: Maintaining Kidney Health
To support optimal kidney function, individuals should adopt lifestyle habits such as:
- Maintaining a balanced diet with adequate hydration
- Regular physical activity without excessive strain
- Avoiding nephrotoxic medications unless prescribed by a doctor
- Undergoing routine kidney function tests, especially for those with underlying risk factors
Understanding the Consequences of Poor Kidney Health
Failing to manage kidney health can lead to severe complications, including the need for dialysis. Dialysis is required when the kidneys lose their ability to filter waste, fluids, and toxins effectively. Key factors leading to dialysis include:
- Chronic Kidney Disease (CKD): Progressive kidney damage from conditions like diabetes and hypertension.
- Acute Kidney Injury (AKI): Sudden loss of kidney function due to infections, dehydration, or toxic exposure.
- End-Stage Kidney Disease (ESKD): Severe kidney failure requiring either dialysis or transplantation.
- Diabetes and Hypertension: Uncontrolled blood sugar and high blood pressure contribute significantly to kidney damage.
- Autoimmune Disorders: Conditions like lupus nephritis can lead to kidney dysfunction.
- Genetic Conditions: Polycystic kidney disease (PKD) and other inherited disorders affect kidney function over time.
Conclusion
Understanding creatinine levels is essential for assessing kidney health and detecting potential issues early. By maintaining a proactive approach to kidney care—including regular monitoring, lifestyle modifications, and medical consultation—individuals can reduce the risk of kidney disease and its severe consequences, such as dialysis. If you are concerned about your kidney health, consult your healthcare provider for further evaluation and management.
Related Resources
- Abnormal Urine pH: What Could It Mean?
- Recurring UTIs: Tests, Reasons & Treatment
- Urinalysis: What Indicates a Urinary Tract Infection (UTI)
- How to Get Rid of a UTI in 24 Hours
References
- Hosten AO. BUN and Creatinine. In: Walker HK, Hall WD, Hurst JW, editors. Clinical Methods: The History, Physical, and Laboratory Examinations. 3rd edition. Boston: Butterworths; 1990. Chapter 193. Available from: https://www.ncbi.nlm.nih.gov/books/NBK305/
- Shahbaz H, Rout P, Gupta M. Creatinine Clearance. [Updated 2024 Jul 27]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2025 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK544228/

Author information not available.


