What Happens When Your Liver Enzymes Are High?
 Written By
Jaclyn P. Leyson-Azuela, RMT, MD, MPH
Written By
Jaclyn P. Leyson-Azuela, RMT, MD, MPH
Many people experience having elevated liver enzymes without symptoms at some point in time. It often triggers asking the question “what happens when your liver enzymes are high”. This often signals temporary issues or conditions that need attention. These enzymes are important markers that help your doctor determine what is happening inside your liver. When levels rise above normal ranges, your liver cells are under stress or experiencing damage. This may sound frightening. But many cases of high liver enzymes are completely reversible with the right approach and lifestyle changes.
This article will explore the causes of high liver enzymes and what you can do to the condition. Understanding what causes these elevations helps you take the right steps toward better liver health. Early detection through regular blood work gives you the best chance for successful treatment and prevents more serious complications.
Key Insights
-
High liver enzymes affect about one-third of Americans and usually indicate treatable conditions like fatty liver disease rather than serious problems
-
Most cases remain completely asymptomatic until advanced stages, making regular blood testing crucial for early detection and prevention
-
Simple lifestyle changes like losing 5-10% of body weight can reduce liver enzymes by 20-30% within 3-6 months
-
Common medications, including acetaminophen and NSAIDs, cause over 50% of drug-induced liver enzyme elevations
-
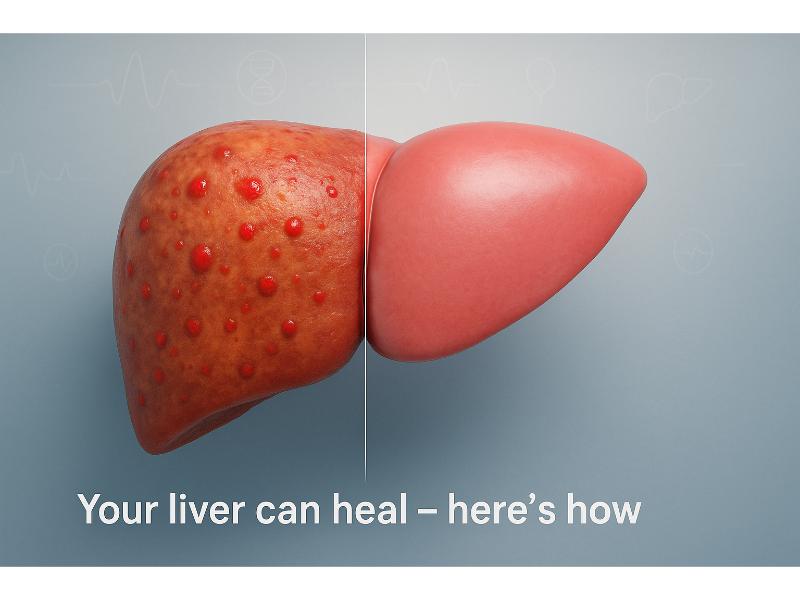
The liver can regenerate damaged tissue when underlying causes are addressed promptly through medical care and lifestyle modifications
What Happens When Your Liver Enzymes Are High?

High liver enzymes signal that your liver cells are releasing more proteins into your bloodstream than usual. This happens when liver cells become damaged or inflamed, causing them to leak their contents into your blood.
Your liver produces several important enzymes that help with digestion, metabolism, and detoxification. The most commonly measured ones include:
-
ALT (alanine aminotransferase) – mainly found in liver cells
-
AST (aspartate aminotransferase) – found in the heart, muscle cells, and the liver
-
ALP (alkaline phosphatase) – found in the bones, bile ducts, and the liver
-
GGT (gamma-glutamyl transferase) – concentrated in the liver and bile ducts
When these enzyme levels climb above the normal ranges, they create a warning signal that something needs attention in your liver. Normal ALT levels stay below 50 IU/L although this depends on the facility where you are undergoing your test. In a study, the reference level for men is between 35-79 IU/L and 31-55 IU/L for women.
Your liver works incredibly hard each day. It processes everything you eat, drink, and breathe. It does the following functions:
-
Filters toxins
-
Produces bile for digestion
-
Stores vitamins
-
Creates protein that your body needs
So, when this vital organ becomes stressed, it releases more enzymes to the blood as the cells become damaged.
Many people worry that high liver enzymes automatically mean serious liver disease. The good news is that temporary elevations often resolve once you address the underlying cause. Your liver has remarkable healing abilities and can regenerate damaged tissue when given proper support.
What Causes High Liver Enzymes?

High liver enzymes often result from liver inflammation or damage. Common causes include fatty liver disease, alcohol use, and medications. According to research, however, about 25% of cases globally are linked to non-alcoholic fatty liver disease (NAFLD) and is one of the leading causes of liver disease in the US.
What Role Do Medications Play in High Liver Enzymes?
Certain medications can temporarily raise liver enzymes by stressing the liver during processing. More than 50% of drug-induced liver issues are caused by common pain relievers like acetaminophen, particularly when combined with alcohol or if consumed in higher doses.
Common medication culprits include:
-
Acetaminophen (safe in normal levels but toxic in excess)
-
NSAIDs (e.g., ibuprofen and naproxen)
-
Statins (e.g., cholesterol medications)
-
Antibiotics
-
Antiseizure drugs
Always inform your doctor about all medications and supplements you take. Many people don’t realize that herbal supplements and over-the-counter (OTC) drugs can also affect liver function. Your pharmacist can help identify potential interactions that may stress your liver.
How Does Fatty Liver Disease Contribute to High Liver Enzymes?
Fatty liver disease builds up fat in liver cells, causing them to leak enzymes into the blood. This condition affects about 1 in 3 US adults (about 30%), making it incredibly common but often undiagnosed.
There are two main types of fatty liver disease exist, including:
-
Alcoholic fatty liver disease (results from excessive alcohol consumption)
-
Non-alcoholic fatty liver disease (NAFLD, occurs without heavy drinking)
NAFLD, now known as Metabolic Dysfunction-Associated Steatotic Liver Disease (MASLD), often develops alongside metabolic syndrome, diabetes, and obesity. The excess fat causes liver cells to become inflamed and damaged over time. Early stages remain reversible through weight loss and dietary changes. But advanced cases can cause scarring (cirrhosis).
Risk factors for MASLD include:
-
Obesity, especially around the midsection
-
Type 2 diabetes or prediabetes
-
High cholesterol or triglycerides
-
Metabolic syndrome
-
Sleep apnea
Losing just 10% or more of your body weight can significantly improve liver enzyme levels and reduce fat accumulation in liver cells.
What Are the Symptoms of Elevated Liver Enzymes?
Many people with high liver enzymes have no symptoms at all. But possible signs include fatigue, jaundice, or abdominal pain. This makes regular blood testing important for early detection, especially if you have risk factors.
Most enzyme elevations remain "silent" in their early stages. Your liver can lose up to 75% of its function before obvious symptoms appear, which explains why many people feel completely normal despite abnormal blood test results.
Common symptoms when they do occur include:
-
Fatigue and weakness
-
Abdominal discomfort
-
Loss of appetite
-
Nausea
-
Dark urine
What Symptoms Indicate Serious Liver Damage?

Serious symptoms like jaundice or leg swelling suggest advanced issues that need immediate medical attention. These warning signs indicate your liver function has become significantly compromised.
Red flag symptoms include:
-
Jaundice
-
Severe abdominal pain
-
Swelling in legs or abdomen
-
Mental confusion
-
Persistent vomiting
-
Easy bruising or bleeding
If you experience any of these symptoms, seek immediate medical care. Early intervention can prevent permanent liver damage and improve your chances of recovery.
How Do High Liver Enzymes Affect Daily Life?
High liver enzymes may cause tiredness that affects work and life activities, even when other symptoms aren’t that obvious or apparent. This fatigue differs from normal daily tiredness from daily activities because no amount of rest can improve it.
People often describe this feeling of tiredness as:
-
Unusual even after doing routine activities
-
Difficulty with concentration particularly at work
-
Less motivation for exercise
-
A need for more sleep than usual
-
“Foggy” or lack of mental clarity
These impacts can affect job performance, relationships, and overall quality of life. Addressing the underlying cause usually restores normal energy levels within weeks to months.
How Are High Liver Enzymes Diagnosed?
Diagnosis starts with blood tests for ALT and AST levels, followed by imaging like ultrasound if needed. Doctors look at enzyme patterns and ratios to determine the most likely causes and next steps.
The diagnostic process typically follows these steps:
-
Medical history review
-
Physical examination
-
Initial blood panel (measures of the basic liver enzymes)
-
Comprehensive metabolic panel (includes the additional liver panel)
-
Additional testing (if initial findings are inconclusive)
What Blood Tests Are Used for Diagnosis?
Key tests measure enzyme levels to identify specific patterns that point toward different causes. Your doctor will look at multiple markers together rather than focusing on single values.
Essential liver function tests include:
-
ALT (normal <50 IU/L)
-
AST (normal <40 IU/L), but levels depend on the facility the usual reference range is 8-33 IU/L
-
ALP (normal 44-147 IU/L)
-
Bilirubin
-
Albumin
-
PT/INR (Tests blood clotting function)
The AST/ALT ratio helps doctors narrow down causes. A ratio above 2:1 often suggests alcohol-related damage, while ratios closer to 1:1 typically indicate other causes like fatty liver disease or medication effects.
When Are Imaging Tests Recommended?
If enzymes stay high after initial treatment, scans check for structural damage or underlying conditions that blood tests might miss. Imaging helps doctors see the liver's size, shape, and internal structure.
Common imaging options include:
-
Ultrasound
-
CT Scan
-
MRI
-
FibroScan
Most healthcare providers start with ultrasound because it is safe, painless, and provides valuable information about liver health. More advanced imaging is reserved for cases where initial tests don’t provide clear answers.
What Treatments Are Available for High Liver Enzymes?
Treatment targets the underlying cause, such as lifestyle changes for fatty liver or stopping problematic medications. There’s no direct “enzyme-lowering” drug because elevated levels are symptoms, not diseases themselves.
Effective treatment approaches include:
-
Identifying and removing causes
-
Lifestyle modifications
-
Managing underlying conditions
-
Regular monitoring
-
Addressing complications
Most people see improvement in 3-6 months when they address the root causes consistently.
How Do Lifestyle Changes Help Treat High Liver Enzymes?

With just achieving 5-10% gradual reduction of body weight, improvement of fatty liver can be achieved within 3-6 months. This represents one of the most effective treatments available, which is possible through sustained weight loss practices.
Proven lifestyle strategies include:
-
Limiting processed foods
-
Regular physical activity
-
Alcohol limitation
-
Adequate hydration
-
Stress management
Weight loss doesn’t have to be dramatic to make a difference. Even modest reductions can significantly improve liver health and enzyme levels over time.
What Medications or Procedures Might Be Needed?
For viral causes like hepatitis, antivirals may be prescribed to reduce liver inflammation and prevent further damage. Treatment depends entirely on the specific underlying conditions that were causing enzyme elevations.
Condition-specific treatments may include:
-
Hepatitis B/C – antiviral medications
-
Autoimmune hepatitis – immunosuppressive drugs
-
Wilson’s disease – copper-binding medications
-
Hemochromatosis – iron reduction through blood removal
-
Severe case – liver biopsy to assess damage extent
Most people won’t need medications or procedures if lifestyle changes successfully address the underlying cause. Your doctor will recommend the least invasive approach first.
How Can You Prevent High Liver Enzymes?
Prevent high liver enzymes by maintaining a healthy weight, limiting alcohol, and getting vaccinated against hepatitis. Prevention is always easier and more effective than treating established liver problems.
Key prevention strategies include:
-
Maintain healthy body weight
-
Exercise regularly
-
Eat a balanced diet
-
Limit alcohol consumption
-
Avoid unnecessary medications
-
Get appropriate vaccinations
-
Practice safe behaviors
What Dietary Changes Prevent High Liver Enzymes?
A balanced diet reduces fat buildup in liver cells and provides nutrients needed for optimal liver function. Focus on foods that support liver health rather than stress this vital organ.
Liver-friendly foods include:
-
Leafy green vegetables
-
Fatty fish
-
Coffee
-
Nuts and seeds
-
Berries
-
Olive oil
Foods to limit or avoid:
-
Highly processed foods
-
Excessive added sugars
-
Trans fats and fried foods
-
Excessive alcohol consumption
How Does Exercise Help in Prevention?
Regular activity burns excess fat stored in liver cells and improves overall metabolic health. The recommended 150 minutes per week of moderate activity can significantly reduce fatty liver disease risk.
Effective exercise options include:
-
Brisk walking
-
Swimming
-
Cycling
-
Resistance training
-
Dancing
You don't need intense workouts to see benefits. Consistent, moderate activity works better than sporadic intense sessions for long-term liver health.
When Should You See a Doctor for High Liver Enzymes?
See a doctor if blood tests show high levels or you have symptoms like jaundice. Early action prevents complications. Don't wait for symptoms to develop, as liver problems often remain silent until advanced stages.
Schedule medical evaluation for:
-
Abnormal blood test results
-
Risk factors present
-
Family history
-
Medication concerns
-
Unexplained symptoms (e.g., fatigue, abdominal pain, nausea)
What Are Warning Signs Requiring Immediate Attention?
Sudden jaundice or confusion needs emergency room evaluation, as these symptoms suggest serious liver dysfunction that could be life-threatening without prompt treatment.
Emergency warning signs include:
-
Yellow skin or eyes
-
Mental confusion
-
Persistent vomiting
-
Swelling in legs or abdomen
-
Easy bruising or bleeding
Don't hesitate to seek emergency care for these symptoms. Quick medical intervention can prevent permanent complications and save lives.
How Often Should You Monitor Liver Enzymes?
Routine checkups catch enzyme elevations early, before symptoms develop or permanent damage occurs. Monitoring frequency depends on your individual risk factors and current health status.
General monitoring guidelines:
-
Low-risk individuals (annual screening or at-home liver tests)
-
Moderate-risk (every six months) – e.g., those obesity, diabetes, family history
-
High-risk (every three months) – e.g., known liver disease, high-risk medications
-
Active treatment – monthly until levels normalize
Regular monitoring allows for early intervention and prevents minor problems from becoming major health issues.
Quick Summary Box
-
High liver enzymes serve as early warning signals that your liver needs attention, but most cases respond well to identifying and treating underlying causes.
-
Whether from fatty liver disease, medications, or other factors, elevated enzyme levels often normalize through weight management, dietary improvements, and medical guidance.
-
Regular monitoring through blood tests catches problems early, while lifestyle changes provide the most effective long-term solutions for maintaining optimal liver health.
References
Agrawal, S., & Khazaeni, B. (2023, June 9). Acetaminophen toxicity. National Library of Medicine; StatPearls Publishing. https://www.ncbi.nlm.nih.gov/books/NBK441917/
ALP. (2024). Rochester.edu. https://www.urmc.rochester.edu/encyclopedia/content?contenttypeid=167&contentid=alkaline_phosphatase
Hallsworth, K., & Adams, L. A. (2019). Lifestyle modification in NAFLD/NASH: Facts and figures. JHEP Reports, 1(6), 468–479. https://doi.org/10.1016/j.jhepr.2019.10.008
Krzysztof Drygalski. (2025). Pharmacological Treatment of MASLD: Contemporary Treatment and Future Perspectives. International Journal of Molecular Sciences, 26(13), 6518–6518. https://doi.org/10.3390/ijms26136518
Laique, S. (2025). Fatty Liver Disease. Cleveland Clinic. https://my.clevelandclinic.org/podcasts/butts-and-guts/fatty-liver-disease
Liver disease in general - The Gut Foundation. (2025, May 8). The Gut Foundation. https://www.thegut.org.nz/know-the-facts/liver/liver-disease-in-general/
Malakouti, M., Kataria, A., Ali, S. K., & Schenker, S. (2017). Elevated Liver Enzymes in Asymptomatic Patients – What Should I Do? Journal of Clinical and Translational Hepatology, 5(4), 394–403. https://doi.org/10.14218/JCTH.2017.00027
Mount Sinai. (n.d.). Aspartate aminotransferase (AST) blood test Information | Mount Sinai - New York. Mount Sinai Health System. https://www.mountsinai.org/health-library/tests/aspartate-aminotransferase-ast-blood-test
Neuschwander-Tetri, B. A. (2008). Influence of Local Reference Populations on Upper Limits of Normal for Serum Alanine Aminotransferase Levels. Archives of Internal Medicine, 168(6), 663. https://doi.org/10.1001/archinternmed.2007.131
Vilar-Gomez, E., Martinez-Perez, Y., Calzadilla-Bertot, L., Torres-Gonzalez, A., Gra-Oramas, B., Gonzalez-Fabian, L., Friedman, S. L., Diago, M., & Romero-Gomez, M. (2015). Weight Loss Through Lifestyle Modification Significantly Reduces Features of Nonalcoholic Steatohepatitis. Gastroenterology, 149(2), 367-378.e5. https://doi.org/10.1053/j.gastro.2015.04.005
World Health Organization. (2023). Physical Activity. World Health Organization. https://www.who.int/initiatives/behealthy/physical-activity
Younossi, Z. M., Golabi, P., Paik, J. M., Henry, A., Van Dongen, C., & Henry, L. (2023). The global epidemiology of nonalcoholic fatty liver disease (NAFLD) and nonalcoholic steatohepatitis (NASH): a systematic review. Hepatology, Publish Ahead of Print(4). https://doi.org/10.1097/hep.0000000000000004

Jaclyn P. Leyson-Azuela, RMT, MD, MPH, is a licensed General Practitioner and Public Health Expert. She currently serves as a physician in private practice, combining clinical care with her passion for preventive health and community wellness.