How Does Toxic Encephalopathy Affect Your Brain—and Can At-Home Tests Help?
 Written By
Jaclyn P. Leyson-Azuela, RMT, MD, MPH
Written By
Jaclyn P. Leyson-Azuela, RMT, MD, MPH
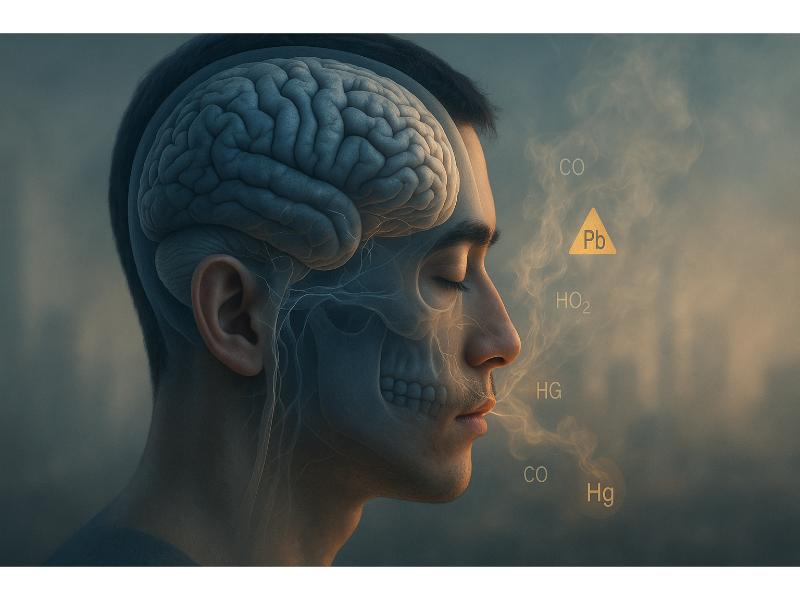
Toxic encephalopathy is a brain dysfunction caused by harmful substances that can damage the brain tissue. The condition develops from exposure to industrial chemicals, heavy metals, medications, or environmental toxins. Symptoms range from mild confusion and memory problems to severe neurological impairment. Early detection through blood tests, urine screening, and imaging helps identify the toxic substance and prevent permanent brain damage.
Key Insights
-
Toxic encephalopathy affects workers in high-risk industries like manufacturing, painting, and chemical production.
-
Brain damage can be reversible if exposure stops early, but chronic exposure may cause permanent cognitive deficits in up to 40 percent of cases.
-
Common workplace toxins include organic solvents like toluene and xylene, heavy metals such as lead and mercury, and carbon monoxide.
-
At-home urine test strips can detect certain heavy metals and drug metabolites, offering preliminary screening before clinical testing.
-
Recovery time varies from weeks to months, with some patients experiencing lingering symptoms like difficulty concentrating and fatigue for over a year.
What Is Toxic Encephalopathy?
Toxic encephalopathy is a brain dysfunction directly caused by toxic substances affecting the brain. The condition develops when neurotoxins cross the blood-brain barrier and can disrupt how the cells work.
The brain is especially vulnerable to toxic substances because it needs constant energy and cannot easily repair damaged neurons. When toxins enter the blood, they accumulate in the brain tissue and cause inflammation, oxidative stress, and cell death. Severity depends on the toxin type, dose, exposure duration, and individual factors.
There are two main types:
-
Acute toxic encephalopathy develops suddenly after a single high-dose exposure or short-term contact with a potent neurotoxin.
-
Chronic toxic encephalopathy results from repeated low-level exposures over months or years, causing gradual brain damage.
The condition affects multiple brain regions. The cerebral cortex controls thinking and memory, and often shows the most damage. The basal ganglia controls movement and can be affected, leading to tremors and coordination problems. The cerebellum may show impairment, causing balance issues and difficulty with fine motor tasks.
How Does Toxic Encephalopathy Develop?
Toxic encephalopathy develops when harmful substances enter the body and travel up to the brain. The toxin may enter through:
-
Breathing
-
Swallowing
-
Skin contact
It could circulate through the bloodstream, cross the blood-brain barrier, accumulate in the brain tissue, and disrupt how cells function.
The blood-brain barrier normally protects the brain from harmful substances, but many industrial chemicals and heavy metals bypass this defense. Lipid-soluble compounds like organic solvents pass through easily. Some metals bind to transport proteins, which will carry them across the membrane. Others, however, cause inflammation that weakens the barrier.
Once inside the brain, toxins interfere with neurotransmitter systems, damage cell membranes, disrupt energy production, and trigger inflammation. The damage builds up over time with repeated exposures.
Who Is at Risk for Toxic Encephalopathy?
Certain groups face higher risk. Workers in specific industries have the greatest exposure risks:
-
Painters and construction workers exposed to solvents and lead
-
Factory workers handling industrial chemicals
-
Agricultural workers using pesticides and herbicides
-
Automotive mechanics working with degreasers and gasoline
-
Welders exposed to metal fumes
-
Dry cleaning employees handling perchloroethylene
Other risk factors include living near industrial sites, using certain medications long-term, having poor nutrition, and having liver or kidney disease.
Children are more vulnerable than adults because their brains are still developing. Older adults face increased risk due to age-related decline in their body's ability to remove toxins.
What Are the First Signs and Symptoms?
The first signs often appear as subtle changes in mental function that gradually worsen. Early symptoms include difficulty concentrating, forgetfulness, mood changes, and fatigue.
Recognizing early warning signs is important because prompt removal from exposure can prevent permanent damage. Many people dismiss initial symptoms as stress or aging, but cognitive decline combined with known toxin exposure should raise concern.
Cognitive and Mental Symptoms
Cognitive symptoms affect thinking, memory, and mental processing:
-
Memory problems, especially difficulty forming new memories or recalling recent events
-
Reduced attention span and inability to focus on tasks
-
Slowed mental processing and delayed responses
-
Confusion about time or place
-
Difficulty with problem-solving and decision-making
-
Language problems, including word-finding difficulty
Mental health symptoms often accompany cognitive changes, including irritability, mood swings, depression, anxiety, personality changes, and reduced emotional control.
Physical and Neurological Symptoms
Physical symptoms indicate nervous system damage. Motor symptoms include:
-
Tremors in the hands or other body parts
-
Poor coordination and clumsiness
-
Muscle weakness
-
Balance problems and abnormal gait
-
Slowed movements
Sensory symptoms affect how the body processes information:
-
Numbness or tingling in hands and feet
-
Vision changes including blurred vision
-
Hearing problems or ringing in the ears
-
Reduced sense of smell or taste
General physical symptoms include persistent headaches, dizziness, nausea, vomiting, fatigue, weakness, sleep disturbances, and loss of appetite.
Symptom Progression Patterns
Symptoms progress in predictable patterns. In acute toxic encephalopathy, symptoms appear suddenly within hours to days. The onset is rapid, symptoms are severe, and you need medical attention immediately.
In chronic toxic encephalopathy, symptoms develop gradually over months or years. Early signs are subtle and easy to miss. Mid-stage symptoms become more noticeable and affect work performance. Late-stage symptoms cause significant disability and may be permanent.
Progression speed depends on:
-
Toxin type
-
Exposure level
-
Individual factors
-
Whether exposure continues
Some patients stabilize after exposure ends. Others continue declining if damage is severe.
What Causes Toxic Encephalopathy?

Toxic encephalopathy results from exposure to substances that damage brain tissue. The causes fall into several categories based on the type of toxic agent.
Understanding specific causes helps identify exposure sources and guide prevention. Each toxin category has distinct exposure routes, risk factors, and symptoms.
Organic Solvents
Organic solvents are among the most common causes of work-related toxic encephalopathy. These chemicals dissolve other substances and are widely used in industry.
Common organic solvents include:
-
Toluene found in paint thinners, adhesives, and gasoline
-
Xylene used in printing, rubber, and leather industries
-
Benzene found in petroleum products and chemical manufacturing
-
Perchloroethylene used in dry cleaning
-
Trichloroethylene used as a degreaser
-
n-Hexane found in glues and varnishes
Workers inhale solvent vapors during daily tasks. The chemicals enter the lungs, pass into the bloodstream, and reach the brain within minutes. Chronic exposure over months or years causes damage.
Solvent-induced encephalopathy affects exposed workers. Symptoms include memory problems, mood changes, coordination difficulties, and slowed thinking. Stopping exposure in early stages often leads to partial recovery.
Heavy Metals
Heavy metals accumulate in the brain and cause persistent damage. The body cannot easily eliminate these substances.
Lead exposure occurs through old paint, contaminated water pipes, industrial settings, and certain ceramics. Lead interferes with neurotransmitter release and damages nerve coverings. Children are especially vulnerable, with exposure causing developmental delays and learning problems. In adults, lead causes memory impairment, mood changes, and nerve damage.
Mercury exposure comes from industrial processes, dental amalgams, and contaminated fish. Methylmercury crosses the blood-brain barrier easily and damages neurons. Symptoms include tremors, vision and hearing changes, coordination problems, and emotional instability.
Manganese toxicity affects welders and miners exposed to metal fumes. Excess manganese accumulates in the basal ganglia and causes Parkinson-like symptoms including tremors, rigidity, slow movements, and psychiatric symptoms.
Other neurotoxic metals include arsenic found in contaminated water and industrial processes, aluminum linked to occupational exposure, and thallium used in manufacturing.
Medications and Drugs
Certain medications cause toxic encephalopathy, especially with prolonged use or in vulnerable patients. Risk increases with higher doses, longer treatment, and impaired drug metabolism.
Medication categories that may cause encephalopathy include:
-
Chemotherapy drugs, particularly methotrexate, cytarabine, and ifosfamide
-
Immunosuppressants like cyclosporine and tacrolimus
-
Certain antibiotics including cephalosporins and fluoroquinolones in high doses
-
Antiepileptic drugs like valproate and phenytoin
-
Lithium used for bipolar disorder
-
Opioid medications in excessive amounts
Substance abuse causes toxic brain damage. Chronic alcohol use leads to vitamin deficiency and direct toxicity. Methamphetamine damages dopamine neurons. Inhalant abuse from huffing causes severe white matter damage.
Environmental and Carbon Monoxide Exposure
Environmental toxins affect both workers and the general population. Carbon monoxide is a colorless, odorless gas produced by incomplete combustion. Sources include faulty heating systems, car exhaust, and fires. Carbon monoxide binds to hemoglobin more strongly than oxygen, depriving the brain of oxygen. Symptoms range from headache and confusion to seizures and coma.
Pesticides and herbicides contain organophosphates and carbamates that block important enzymes. Agricultural workers and those living near farms face exposure risk. Symptoms include confusion, memory problems, mood changes, and autonomic dysfunction.
Industrial chemicals like cyanide, hydrogen sulfide, and various plasticizers can cause acute or chronic toxicity through workplace accidents or environmental contamination.
Risk Factors That Increase Susceptibility
Individual factors affect how likely someone is to develop toxic encephalopathy. Genetic variations mean some people process toxins less efficiently. Pre-existing medical conditions like liver disease or kidney problems impair toxin elimination. Nutritional deficiencies reduce antioxidant protection. Age affects vulnerability, with children and older adults at higher risk. Exposure to multiple toxins creates additive effects.
How Is Toxic Encephalopathy Diagnosed?
Diagnosing toxic encephalopathy requires a comprehensive approach combining:
-
Medical history
-
Physical examination
-
Laboratory testing
-
Brain imaging
The process confirms brain dysfunction, identifies the toxic substance, and rules out other conditions.
Accurate diagnosis is essential because many conditions cause similar symptoms. The evaluation typically takes several days to weeks as results become available.
Medical History and Physical Examination
The diagnostic process starts with a detailed medical history. Your doctor will ask about work exposures, including job duties, chemicals handled, and workplace safety measures. Environmental exposures like home location, hobbies, and recent renovations are reviewed. All medications, supplements, and recreational substances are documented. Symptom timing helps establish when exposure occurred.

The physical examination includes a neurological assessment. Your doctor tests mental status, memory, attention, and language. Coordination and balance are evaluated through specific movement tests. Reflexes are checked. Cranial nerve function is assessed. Sensory testing identifies areas of numbness.
Blood tests identify specific toxins and check organ function:
-
Complete blood count to check for anemia or blood disorders
-
Metabolic panel to evaluate liver and kidney function
-
Heavy metal levels for lead, mercury, arsenic, and other metals
-
Drug screens to detect medications or substances of abuse
Specialized tests may include enzyme levels if pesticide exposure is suspected, carboxyhemoglobin for carbon monoxide poisoning, and vitamin levels, particularly B12 and thiamine.
Urine testing complements blood work. Urine tests can detect heavy metals, drug metabolites, and organic acid metabolites from solvent exposure. Twenty-four hour urine collections provide more accurate measurements than single samples. At-home urine test strips also provide some form of screening if kidney function needs to be evaluated.
Brain Imaging Studies
Imaging helps visualize brain damage and rule out other causes. MRI scans are the most sensitive imaging test. MRI can show white matter changes from solvent exposure, basal ganglia abnormalities from metal toxicity, and areas of brain shrinkage.
Specific MRI findings depend on the toxin. Carbon monoxide poisoning shows damage to the globus pallidus. Methanol toxicity affects the putamen. Chronic solvent exposure causes diffuse white matter changes.
CT scans are faster and more available than MRI but less sensitive for subtle changes. CT scans are useful for ruling out stroke, bleeding, or tumors but may appear normal in early toxic encephalopathy.
Neuropsychological Testing
Formal cognitive testing measures specific mental functions affected by toxic exposure. Tests evaluate memory (short-term and long-term), attention and concentration, processing speed, problem-solving, language abilities, and visual-spatial skills.
Testing typically takes 2 to 4 hours. Results are compared to age and education-matched norms. The pattern of deficits helps distinguish toxic encephalopathy from other conditions like Alzheimer disease or depression.
Can You Test for Toxins at Home?
At-home urine test strips offer a preliminary screening option for certain toxic substances. These tests detect specific toxins or their metabolites in urine samples collected at home.
Home testing serves as an early warning system for people with known exposure risks. The tests cannot diagnose toxic encephalopathy but can identify elevated toxin levels that need further medical evaluation.
Types of At-Home Urine Tests
Several categories of at-home tests are available. Heavy metal tests screen for lead, mercury, arsenic, and cadmium. You collect a urine sample, mail it to a laboratory, and receive results within days. These tests are useful for people living in older homes with lead pipes or those with work-related exposure to metals.
Drug screening tests detect medications and substances of abuse. Tests identify opioids, benzodiazepines, amphetamines, and other drugs. Results appear within minutes. These tests help monitor medication compliance or detect substance use.
Some specialized tests screen for organic solvent metabolites. These are less common but available for workplace health monitoring.
Simple urine test strips can also detect proteins or substances that imply damage to the filtering capacity of the kidneys.
How to Use At-Home Urine Test Strips
Using home test strips involves several steps:
-
Read all instructions from the product label before starting
-
Collect a urine sample in a clean, sterile container
-
Dip the test strip in the sample for a specified time as instructed
-
Wait for the indicated development time
-
Compare the strip colors to the chart provided or via the app on your smartphone (if included in the subscription)
-
Record your results
Timing matters. First morning urine often contains the highest toxin concentration. Some tests require avoiding certain foods or supplements before testing. Follow all instructions to ensure accurate results.

What At-Home Tests Can and Cannot Detect
At-home tests have specific capabilities and limitations. Tests can detect the presence of certain heavy metals and drug metabolites, identify exposure levels above normal ranges, and provide trend data when used repeatedly over time.
Tests cannot diagnose toxic encephalopathy or other medical conditions, detect all toxic substances, measure brain damage or cognitive impairment, or replace comprehensive medical evaluation.
False positives occur from certain foods, medications, or supplements. False negatives happen when toxin levels fall below detection limits or the wrong test is used. Results need confirmation by clinical laboratory testing.
Accuracy and Reliability
Test accuracy varies by brand and substance tested. Heavy metal tests are generally sensitive compared to clinical laboratory testing. Drug screening tests range from 90 to 99 percent accurate for most substances.
Factors affecting accuracy include sample collection technique, timing of collection relative to exposure, proper storage before testing, and correct interpretation of results. Clinical confirmation is essential before making health decisions based on home test results.
Cost and Accessibility
At-home urine test strips cost depend on the number of substances tested. Single-use strips are cheapest; multi-substance panels cost more. Tests requiring lab analysis add shipping and processing fees.
Most are sold online or in pharmacies without a prescription. Insurance rarely covers home tests, though follow-up clinical tests may be covered if results are abnormal.
When to Choose At-Home Testing
Home testing is useful if you:
-
Work in high-risk environments
-
Want to monitor exposure time or track recovery
-
Live in contaminated areas
-
Need preliminary screening before a medical visit
Avoid home testing if:
-
Symptoms are severe or worsening
-
Immediate medical care or official diagnosis is needed
-
Complex or comprehensive toxin screening is required
Benefits for Specific Groups
-
Industrial workers: Monitor chronic exposures
-
Parents: Screen children for lead
-
Older adults: Check for heavy metals in homes with old plumbing
-
Patients on risky medications: Track drug levels
-
Recovering individuals: Monitor ongoing improvement
What Treatments and Recovery Options Exist?
Treatment for toxic encephalopathy focuses on stopping the exposure, removing the toxin from the body when possible, managing symptoms, and supporting brain recovery through rehabilitation. The approach depends on the specific toxin, symptom severity, and how quickly treatment begins.
Early intervention improves outcomes. The brain has some capacity to heal and compensate for damage, especially when exposure stops promptly.
Removing the Exposure Source
The first step is stopping contact with the toxin. For work exposures, this may mean leaving the job, using protective gear, improving ventilation, and following OSHA limits.
For environmental causes, move away from contaminated areas, fix sources like lead pipes, dispose of toxic materials properly, and improve ventilation.
If medication-related, your doctor will stop or replace the drug and adjust doses as needed.
Medical Interventions
Treatment focuses on removing toxins and managing symptoms. Chelation therapy with agents like EDTA, DMSA, or dimercaprol removes heavy metals (lead, mercury, arsenic) and requires multiple sessions.
Supportive care may include seizure control, tremor management, antidepressants, and cognitive enhancers.
Severe cases may need hemodialysis (for lithium or methanol), hyperbaric oxygen (for carbon monoxide), or intensive care.
Rehabilitation Therapies
Rehabilitation restores function and teaches coping skills.
-
Cognitive therapy improves memory, attention, and problem-solving through exercises and compensatory strategies
-
Physical therapy builds strength, balance, and coordination, may use assistive devices
-
Occupational therapy re-teaches daily and work tasks, adapts environments for safety
-
Speech therapy addresses communication and swallowing issue
Nutritional Support
Balanced nutrition aids brain healing. Antioxidants (vitamins C, E), B vitamins, omega-3s, and protein support recovery. Supplements like NAC, alpha-lipoic acid, and milk thistle may help but should be discussed with a doctor.
Recovery Timeline and Prognosis
Recovery depends on toxin type, exposure duration, health, and brain injury severity.
-
Acute cases often improves in weeks to months with mild cases may be able to fully recover
-
Chronic cases improve slowly over months to years. Some deficits may remain. Better outcomes occur with early treatment, milder symptoms, and consistent rehab.
Long-Term Monitoring
Follow-up includes neurological exams, cognitive tests, toxin level checks, and imaging as needed.
Mild cases need visits every 3–6 months; severe cases may require monthly reviews early on.

Preventing Recurrence
Avoid re-exposure through protective equipment, job or lifestyle changes, home testing, and regular medication reviews. Learn toxin sources and early warning signs.
Support and Resources
Resources include occupational health clinics, neuropsychologists, social workers, support groups, and vocational rehab. Disability benefits, workers’ compensation, or legal aid may apply for severe or work-related cases.
Related Resources
Is F3 Liver Fibrosis Reversible?
Can You Get Disability for Cirrhosis of The Liver?
Quick Summary Box
-
Toxic encephalopathy is brain dysfunction caused by harmful substances that damage nerve cells and disrupt normal brain function.
-
Common causes include organic solvents, heavy metals (lead, mercury), medications, carbon monoxide, and pesticides.
-
Key symptoms include memory problems, confusion, difficulty concentrating, tremors, coordination issues, mood changes, and fatigue.
-
Diagnosis may involve medical history, neurological exam, blood and urine tests, brain imaging (MRI/CT), and cognitive testing.
-
Urine test strips can detect certain heavy metals and drugs but cannot diagnose the condition or replace comprehensive medical evaluation.
-
Treatment should be focused on stopping the exposure, chelation therapy for metals, symptom management, and rehabilitation (cognitive, physical, occupational therapy).
-
Recovery varies from weeks to years depending on toxin type, exposure duration, and treatment timing. Early intervention improves outcomes.
-
Use protective equipment at work, test home environments for toxins, avoid unnecessary medication use, and monitor high-risk exposures.
References
Chue, A. L., Fernando, I. N., Hussain, S. A., & Yates, D. A. (2009). Chemotherapy related encephalopathy in a patient with Stage IV cervical carcinoma treated with cisplatin and 5-fluorouracil: a case report. Cases Journal, 2(1), 8526. https://doi.org/10.4076/1757-1626-2-8526
Council, R., Russell, R. W., Flattau, P. E., & Pope, A. M. (2025). Methods and Issues in Evaluating the Neurotoxic Effects of Organic Solvents. Nih.gov; National Academies Press (US). https://www.ncbi.nlm.nih.gov/books/NBK234987/
Del Prado-Lu, J. (2007). Pesticide exposure, risk factors and health problems among cutflower farmers: a cross sectional study. Journal of Occupational Medicine and Toxicology, 2(1), 9. https://doi.org/10.1186/1745-6673-2-9
Evans, G. R., & Masullo, L. N. (2021). Manganese Toxicity. PubMed; StatPearls Publishing. https://www.ncbi.nlm.nih.gov/books/NBK560903/
Graham, J., & Traylor, J. (2023, February 13). Cyanide Toxicity. Nih.gov; StatPearls Publishing. https://www.ncbi.nlm.nih.gov/books/NBK507796/
Kim, Y., & Kim, J. W. (2012). Toxic Encephalopathy. Safety and Health at Work, 3(4), 243–256. https://doi.org/10.5491/shaw.2012.3.4.243
Kinoshita, T., Sugihara, S., Eiji Matsusue, Fujii, S., Motoki Ametani, & Ogawa, T. (2005). Pallidoreticular Damage in Acute Carbon Monoxide Poisoning: Diffusion-Weighted MR Imaging Findings. AJNR: American Journal of Neuroradiology, 26(7), 1845. https://pmc.ncbi.nlm.nih.gov/articles/PMC7975158/
Macchi, Z. A., Carlisle, T. C., & Filley, C. M. (2022). Prognosis in substance abuse-related acute toxic leukoencephalopathy: A scoping review. Journal of the Neurological Sciences, 442, 120420. https://doi.org/10.1016/j.jns.2022.120420
Mahaffey, K. R. (2024). Mercury Exposure: Medical and Public Health Issues. Transactions of the American Clinical and Climatological Association, 116, 127. https://pmc.ncbi.nlm.nih.gov/articles/PMC1473138/
Mamera, M., van Tol, J. J., Aghoghovwia, M. P., & Kotze, E. (2020). Sensitivity and Calibration of the FT-IR Spectroscopy on Concentration of Heavy Metal Ions in River and Borehole Water Sources. Applied Sciences, 10(21), 7785. https://doi.org/10.3390/app10217785
Mandiga, P., Foris, L. A., Kassim, G., & Bollu, P. C. (2025, January 20). Hepatic Encephalopathy. National Library of Medicine; StatPearls Publishing. https://www.ncbi.nlm.nih.gov/books/NBK430869/
Pervin, Z., & Stephen, J. M. (2021). Effect of alcohol on the central nervous system to develop neurological disorder: pathophysiological and lifestyle modulation can be potential therapeutic options for alcohol-induced neurotoxication. AIMS Neuroscience, 8(3), 390–413. https://doi.org/10.3934/neuroscience.2021021
Valk, J., & van der Knaap, M. (1992). Toxic encephalopathy. https://www.ajnr.org/content/ajnr/13/2/747.full.pdf
World Health Organization. (2024). Lead Poisoning and Health. Who.int; World Health Organization: WHO. https://www.who.int/news-room/fact-sheets/detail/lead-poisoning-and-health
Xavier, C., Kuo, M., Desai, R., Palis, H., Regan, G., Zhao, B., Moe, J., Scheuermeyer, F., Wen Qi Gan, Sabeti, S., Meilleur, L., Buxton, J. A., & Slaunwhite, A. (2023). Association between toxic drug events and encephalopathy in British Columbia, Canada: a cross-sectional analysis. Substance Abuse Treatment Prevention and Policy, 18(1). https://doi.org/10.1186/s13011-023-00544-z

Jaclyn P. Leyson-Azuela, RMT, MD, MPH, is a licensed General Practitioner and Public Health Expert. She currently serves as a physician in private practice, combining clinical care with her passion for preventive health and community wellness.



