Liver Laceration: What It Means, How It's Treated, and What Recovery Looks Like
 Written By
Abel Tamirat, MD
Written By
Abel Tamirat, MD
If you've experienced a blow to the abdomen, your liver could be more affected than you think. Liver lacerations—tears in the liver tissue—are among the most common internal injuries after blunt trauma. You might not feel symptoms right away, but signs like abdominal pain, shoulder aches, or unexplained fatigue could point to something more serious.
This isn’t just a bruise or a pulled muscle. A liver laceration can lead to internal bleeding, organ damage, or long-term complications if left untreated. At the same time, your body has an incredible ability to heal—especially with the right support and medical care.
In this guide, you’ll get a clear understanding of what a liver laceration is, how it happens, and how it’s treated.
What is a liver laceration?
A liver laceration is a tear or cut in the tissue of your liver. It usually results from trauma—most commonly blunt abdominal injuries, such as:
-
Motor vehicle accidents
-
Falls
-
Sports injuries
-
Violence or assault (e.g. stabbing or gunshot wounds)
Depending on the severity, a laceration can cause minor bleeding or lead to a life-threatening internal hemorrhage. The liver is a highly vascular organ, meaning it has many blood vessels. Even a small tear can result in significant blood loss.
Learn more about liver pain location and its symptoms to better understand how trauma may present.
Why is the liver prone to injury?
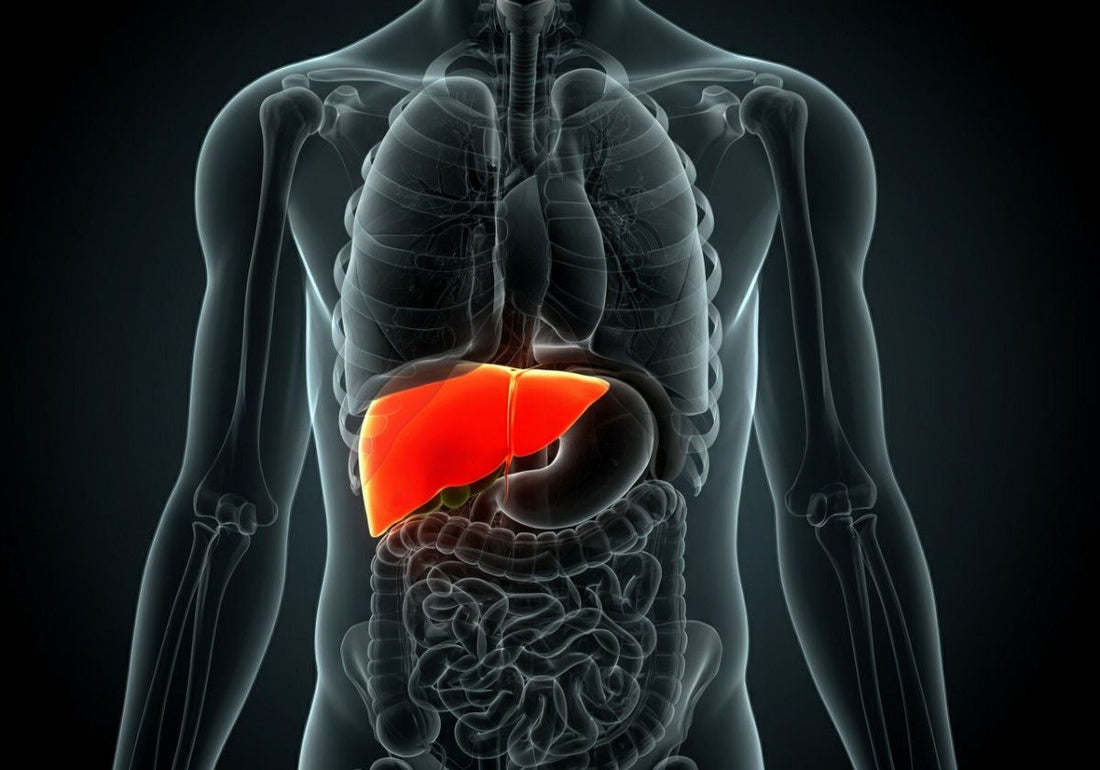
The liver is the largest solid organ in the body, sitting in the upper right part of your abdomen, just beneath the ribcage. While the ribs provide some protection, the liver is still vulnerable to forceful impacts due to:
-
Its large size
-
Its soft, spongy texture
-
Its high blood content
Unlike muscles or bones, the liver doesn't have strong structural resistance to trauma. That’s why liver injuries are among the most common abdominal injuries in trauma cases.
For more information on long-term health, see our guide on signs your liver is healing.
How are liver lacerations classified?
Liver lacerations are graded from I to VI based on the American Association for the Surgery of Trauma (AAST) liver injury scale:
Grade I–II (Mild)
-
Small tears (under 3 cm deep)
-
Minor bleeding
-
Often managed without surgery
Grade III (Moderate)
-
Deeper tears (more than 3 cm)
-
May include active bleeding
-
Observation or minimally invasive treatment may be required
Grade IV–V (Severe)
-
Extensive tears involving multiple lobes
-
Injury to major blood vessels
-
Often requires surgical repair or intervention
Grade VI (Critical)
-
Hepatic avulsion (complete separation of the liver from blood supply)
-
Rare and often fatal without immediate emergency surgery
What causes a liver laceration?

Most liver lacerations are caused by blunt trauma, such as:
-
Car crashes
-
High falls (especially onto hard surfaces)
-
Contact sports injuries
-
Bicycle accidents
-
Assault
Penetrating trauma (like stab or gunshot wounds) can also cause liver tears, often more severe and complex to treat.
In rare cases, medical procedures (such as liver biopsies or surgeries) may unintentionally result in a liver laceration, although this is uncommon.
Because the liver is large and vascular, it’s also a common site for conditions such as liver cysts or even liver lesions unrelated to trauma.
What symptoms suggest a liver laceration?
The signs can vary depending on how severe the tear is. Some people may feel only mild pain, while others experience intense symptoms.
Common signs include:
-
Pain or tenderness in the upper right abdomen
-
Shoulder pain (especially right-sided, from referred pain)
-
Swelling or bruising on the right side of the torso
-
Nausea or vomiting
-
Dizziness or lightheadedness (from internal bleeding)
-
Low blood pressure or rapid heart rate
-
Pale or cool skin
-
Fatigue or confusion
Severe bleeding can lead to shock, which is a medical emergency.
If someone shows signs of low blood pressure, rapid breathing, or confusion after abdominal trauma, seek emergency care immediately.
If you’re not sure what liver pain feels like, here’s a breakdown of what can be mistaken for liver pain.
How is a liver laceration diagnosed?
Doctors typically use a combination of physical exams and imaging tests to confirm a liver injury.
1. Physical Exam
-
Doctors will check for tenderness, swelling, or signs of internal bleeding.
-
They may ask about the accident or impact that caused the injury.
2. Focused Assessment with Sonography for Trauma (FAST)
-
FAST is a bedside ultrasound used to detect internal bleeding quickly.
3. CT Scan (Computed Tomography)
-
This is the most reliable way to diagnose a liver laceration.
-
It shows the size, depth, and location of the tear and any active bleeding.
4. MRI or Angiography (less common)
-
These may be used if a CT scan is inconclusive or if there’s suspected vascular injury.
How is a liver laceration treated?
Treatment depends heavily on the severity (grade) of the laceration and whether there’s active bleeding.
Mild (Grades I–II)
-
Typically managed non-surgically in the hospital
-
Monitoring for internal bleeding
-
Pain management
-
Rest and restricted activity
Moderate (Grade III)
-
Observation plus interventional radiology (e.g., embolization to stop bleeding)
-
Hospital stay may last several days
Severe (Grades IV–V)
-
May require surgery to repair the liver or stop bleeding
-
Intensive care monitoring
-
Blood transfusions if necessary
Critical (Grade VI)
-
Requires immediate life-saving surgery
-
May involve liver resection (removal of damaged portion)
-
Rarely, a liver transplant is needed in catastrophic cases
Can a liver laceration heal on its own?
Yes—in many mild and moderate cases, the liver can heal without surgery. The liver has a remarkable ability to regenerate and repair itself over time.
Recovery depends on:
-
The extent of the injury
-
How well bleeding is controlled
-
Your overall health
-
Proper rest and follow-up care
Even after healing, your liver may have scar tissue. This doesn’t usually impair function but may require monitoring in the future.
Supporting recovery is key. You may want to explore the best vitamins for liver health or ask, what vitamins help liver repair?
What does liver laceration recovery involve?
Recovery from a liver laceration can take weeks to several months, depending on the severity. Here's what to expect:
In the hospital:
-
Monitoring vital signs and blood levels
-
Imaging to track healing
-
IV fluids and pain relief
-
Bed rest, especially during the first 24–72 hours
At home:
-
Gradual return to activity—usually within 4–6 weeks for mild injuries
-
Avoid heavy lifting, contact sports, or straining for at least 6–8 weeks
-
Attend all follow-up visits
-
Maintain a healthy, nutrient-rich diet to support liver regeneration
What complications can arise?
Though most people recover well, complications are possible—especially with severe injuries. These include:
-
Hemorrhage (continued or recurrent bleeding)
-
Infection or abscess in the liver
-
Bile leak from damaged ducts
-
Scar tissue or fibrosis
-
Liver failure (rare, but possible in major injuries)
Any new or worsening symptoms—such as fever, abdominal swelling, yellowing of the eyes, or ongoing pain—should be evaluated promptly.
Can children get liver lacerations?
Yes. Children are particularly vulnerable to liver injuries due to:
-
Smaller body size
-
Less abdominal fat and protection
-
More elastic ribs that bend without breaking
Fortunately, most pediatric liver injuries can be treated non-surgically, and children tend to heal faster than adults. But close monitoring is still essential.
How can you support liver healing after injury?
If you're recovering from a liver laceration—or helping someone who is—small lifestyle adjustments can support healing:
1. Stay hydrated
Drink water regularly. Proper hydration supports circulation and tissue healing.
2. Eat a liver-friendly diet
Try a liver-friendly diet that promotes healing, that focuses on:
-
High-protein foods (chicken, legumes, tofu)
-
Leafy greens (spinach, kale)
-
Antioxidant-rich fruits (berries, citrus)
-
Whole grains (brown rice, oats)
Avoid:
-
Avoid alcohol – see how much alcohol is in beer and how it affects your recovery
-
High-fat, fried, or heavily processed foods
-
Added sugars and sodas
Consider testing your liver at home with the Ribbon Liver Test
3. Follow your doctor’s advice
Don’t resume exercise or sports until you get medical clearance—even if you feel better.
4. Get enough sleep
Your body needs rest to repair tissue, especially your liver, which does much of its regeneration at night.
5. Avoid unnecessary medications
Check with your doctor before using any over-the-counter meds or supplements, especially acetaminophen, which can strain your liver.
Can you prevent liver lacerations?

While accidents are sometimes unavoidable, you can reduce your risk:
-
Always wear a seatbelt
-
Use protective gear during sports (helmets, padding)
-
Avoid risky physical behavior (e.g., jumping from high places)
-
Secure your home to prevent falls, especially for children or older adults
When should you seek help?
You should go to the emergency room if:
-
You’ve experienced abdominal trauma (even if pain seems minor)
-
You feel dizzy, faint, or confused
-
Your skin looks pale or clammy
-
Your abdomen becomes swollen or very tender
-
You have ongoing pain in your upper right side or shoulder
If you’ve already been diagnosed with a liver laceration and notice new or worsening symptoms, reach out to your care team immediately.
Can you live a normal life after a liver laceration?
Yes. Many people go on to live full, active lives after recovering from a liver injury—especially if it was treated properly and no major complications occurred.
The key is giving your body the time and resources it needs to heal. That includes physical rest, emotional support, and healthy habits that prioritize liver function.
Learn about detoxing your liver safely and whether non-alcoholic beer is safe for your liver.
Key takeaways: What should you remember about liver lacerations?
-
A liver laceration is a tear in the liver, often caused by blunt or penetrating trauma.
-
Symptoms include upper abdominal pain, bruising, shoulder pain, and signs of internal bleeding.
-
Diagnosis is made via CT scan, and treatment depends on severity, from observation to surgery.
-
Most mild injuries heal on their own, while severe cases may need surgical intervention.
-
Recovery takes time, rest, and follow-up care—but full healing is often possible.
Looking to monitor your liver health?
Explore Ribbon Checkup’s at-home liver test kits and get insights without leaving home. Or sign up for our newsletter for monthly liver health updates.
Related Resources
At-Home Liver Tests: A Comprehensive Guide
Inflamed Liver Treatment: Expert Advice on Effective Management Options
Which Painkiller Is Safe for the Liver?
References
Ahmed, N., & Vernick, J. (2011). Management of liver trauma in adults. Journal of Emergencies, Trauma, and Shock, 4(1), 114. https://doi.org/10.4103/0974-2700.76846
Coccolini, F., Coimbra, R., Ordonez, C., Kluger, Y., Vega, F., Moore, E. E., … Maier, R. (2020). Liver trauma: WSES 2020 guidelines. World Journal of Emergency Surgery, 15(1). https://doi.org/10.1186/s13017-020-00302-7
Levent Kaptanoglu, Kurt, N., & Hasan Ediz Sikar. (2017). Current approach to liver traumas. International Journal of Surgery, 39, 255–259. https://doi.org/10.1016/j.ijsu.2017.02.015
Nall, R. (2020, March 30). Bruised Liver. Retrieved July 12, 2025, from Healthline website: https://www.healthline.com/health/liver-punch
Taghavi, S., & Askari, R. (2023, July 17). Liver Trauma. Retrieved July 12, 2025, from Nih.gov website: https://www.ncbi.nlm.nih.gov/books/NBK513236/
UpToDate. (2025). Retrieved July 12, 2025, from Uptodate.com website: https://www.uptodate.com/contents/management-of-hepatic-trauma-in-adults
O’Rourke, M. C., Landis, R., & Burns, B. (2023, July 24). Blunt Abdominal Trauma. Nih.gov; StatPearls Publishing. https://www.ncbi.nlm.nih.gov/books/NBK431087/
Marietta, M., & Burns, B. (2025, February 15). Penetrating Abdominal Trauma. Nih.gov; StatPearls Publishing. https://www.ncbi.nlm.nih.gov/books/NBK459123/

Dr. Abel Tamirat is a licensed General Practitioner and ECFMG-certified international medical graduate with over three years of experience supporting U.S.-based telehealth and primary care practices. As a freelance medical writer and Virtual Clinical Support Specialist, he blends frontline clinical expertise with a passion for health technology and evidence-based content. He is also a contributor to Continuing Medical Education (CME) programs.


