Can Liver Disease Cause Headaches? Knowing The Connection and Safe Liver Disease Headache Treatment
 Written By
Jaclyn P. Leyson-Azuela, RMT, MD, MPH
Written By
Jaclyn P. Leyson-Azuela, RMT, MD, MPH
The liver is an important organ, playing a critical role in maintaining your overall health. But, if it fails, the cascade of issues can potentially come up and be a problem of the entire body instead. Among these potential issues, headaches can emerge as really surprising but no matter how minor it sounds, it can often be debilitating. It may be an indicator that an underlying liver dysfunction is affecting you.
Knowing the intricate connection between liver health and headaches is essential for efficient management and improved well-being. The article explores how liver disease can manifest as headaches, understanding the mechanisms, types, and available treatment options.
Key Insights
-
Liver disease may cause headaches, particularly through hepatic encephalopathy, where toxins like ammonia affect brain function.
-
Research suggests a possible link between migraines and non-alcoholic fatty liver disease (NAFLD), but evidence is limited and requires further study.
-
Treatment focuses on managing liver conditions with medications like lactulose and using safe pain relievers like low-dose acetaminophen.
-
Natural remedies and lifestyle changes, such as a liver-friendly diet and avoiding alcohol, can support liver health and reduce headaches.
-
Consulting a healthcare provider for persistent headaches or liver disease symptoms is critical for early diagnosis.
What Is Liver Disease and How Does It Affect the Body?
Functions of the liver
Liver disease refers to any condition that can damage that liver and prevents it from working as it should. The liver is located in the upper right part of the abdomen. It performs various essential tasks, including:
-
Filtering toxins from your blood
-
Producing proteins that are necessary for blood to clot
-
Aiding in digestion
But when the liver is compromised, these critical functions can alter significantly, which leads to a wide range of health problems through the body.
What are the common causes of liver disease?
Several factors can contribute to liver damage. It could range from viral infections to lifestyle choices. Some of the most common causes include:
-
Viral hepatitis–hepatitis B and C infections are significant contributors to liver disease. Hepatitis C, specifically, affects about 2.4 million Americans. These viruses can cause swelling of the liver, which if left untreated, can lead to severe damage over-time
-
Chronic alcohol use–alcohol consumption in excess is one of the leading causes of liver diseases. It can progress to fatty liver and may become alcoholic hepatitis and eventually cirrhosis. Alcohol-related liver disease accounts for about 5.1% global burden and is a significant cause of liver-related deaths in the US.
-
Non-Alcoholic Fatty Liver Disease (NAFLD)–now referred to as metabolic dysfunction-associated steatotic liver disease (MASLD), and is characterized by fat buildup in the liver in people who drink little or no alcohol. It is increasingly prevalent, which affects an estimated 24% of adults in the US. NAFLD can progress to non-alcoholic steatohepatitis (NASH), which is a more severe form that involves inflammation and liver cell damage.
-
Genetic disorders–inherited conditions like hemochromatosis (iron overload) and Wilson’s disease (copper buildup) can lead to liver damage, as well.
-
Autoimmune diseases–these are conditions when the body’s immune system attacks the liver, leading to autoimmune hepatitis
How does liver disease typically progress?
Liver disease often develops in stages, with damage accumulating over time. Knowing these stages can help in recognizing the severity of the condition:
-
Inflammation–the initial stage where the liver becomes inflamed due to injury or infection. At this point, the symptoms may be subtle or even non-existent.
-
Fibrosis–the persistence of inflammation leads to fibrosis, where there is scarring. The scarring is known as fibrosis, which replaces healthy liver tissue, but it does not signify impairment of liver function just yet
-
Cirrhosis–is a more advanced stage, where there is extensive scarring. It severely impacts the liver’s ability to function. Cirrhosis is irreversible and can lead to liver failure. This is a major cause of death in the US.
-
End-stage liver disease (ESLD)–the liver is severely damaged at this point and can no longer perform its essential functions. ESLD may lead to complications, including liver cancer or the need for a liver transplant.
How Can Liver Disease Lead to Headaches?

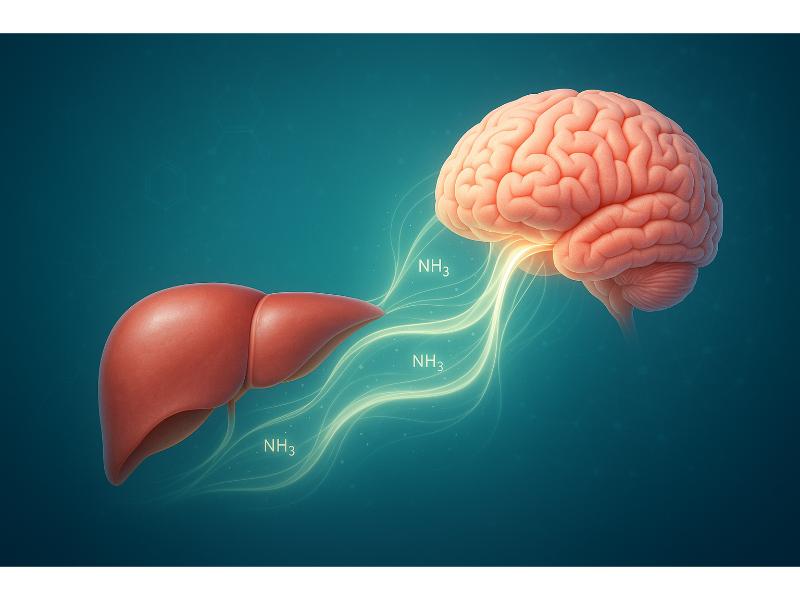
When your liver is struggling and isn’t working properly, its function is compromised, including the function of filtering out harmful substances from the blood. The toxins can accumulate and travel to your brain, which will manifest with neurological symptoms like headaches. The connection is particularly evident in a condition called hepatic encephalopathy (HE), where the brain function is affected because of liver compromise.
What happens to your brain when your liver isn't functioning well?
The liver is a powerful filter that’s able to clean your blood of waste products and toxins. But when it is not doing its job effectively, the harmful substances, especially ammonia, can accumulate in the blood. The blood-brain barrier (BBB), which is the brain’s coating, normally protects your brain from harmful substances that can be compromised following liver disease. The toxins can cross the BBB and into the brain, which interferes with brain cell communication and function. It leads to neurological symptoms, such as:
-
Confusion
-
Disorientation
-
Headaches
What role does ammonia play in liver disease headaches?
Ammonia is a byproduct of protein digestion, which is normally converted into urea by a healthy liver before it gets excreted by the kidneys. For individuals with liver disease, the conversion process is impaired that leads to increased levels of ammonia in the blood.
High ammonia levels are a key factor for the development of hepatic encephalopathy. While not all elevated ammonia levels can directly cause HE, they are strong indicators of liver dysfunction leading to neurological symptoms, which in this case is headache. High ammonia levels are frequently seen in hepatic encephalopathy but they are not often required for its development.
What Types of Headaches Are Associated with Liver Disease?
Headaches linked to liver disease can vary, but they often include tension-type headaches or those directly related to hepatic encephalopathy. There’s also research that explores a potential link between migraines and non-alcoholic fatty liver disease (NAFLD).
Is there a link between migraines and liver health?
Like mentioned, there is research suggesting the link between migraines and liver health, particularly NAFLD. There are also some that state patients with migraine and NAFLD may experience more frequent attacks. The exact mechanism why this is happening is still unknown, but inflammation and metabolic factors, which are common denominators of both conditions, are thought to play a role. The evidence is still limited as of date and more research is necessary to establish the link. But the systemic nature of liver health can have far-reaching effects on the body.
What do headaches from hepatic encephalopathy feel like?
Headaches that are associated with HE often occur alongside other neurological symptoms, including:
-
Confusion
-
Fatigue
-
Changes in personality
-
Difficulty concentrating
These headaches are not always distinct in their characteristics, meaning they might not have a specific pattern that will set them differently from other types of headaches. Rather, they are part of a broader spectrum of brain dysfunction that is caused by the liver’s impaired ability to process and remove toxins. It is important that the headache is recognized as a result of the liver’s dysfunction, especially when it is accompanied by other symptoms. But it is important to establish that you have a known liver issue first.
When Should You See a Doctor for Liver Disease-Related Headaches?
It’s important to seek medical care if you’re experiencing a persistent headache, especially if it is associated with other symptoms. It could indicate that you may be having some liver problems. Early detection and intervention are essential to manage liver disease effectively.
What symptoms indicate that headaches might be related to liver disease?

Headaches have many causes, but if it is associated with other symptoms, it should prompt you to seek medical evaluation right away. The red flags could include:
-
Jaundice
-
Persistent fatigue
-
Abdominal swelling (could be associated with ascites)
-
Abdominal pain (feeling bloated and dull discomfort in the upper right abdomen)
-
Dark urine
-
Pale stools
-
Nausea
-
Vomiting
-
Easy bruising
-
Bleeding
-
Confusion or disorientation
-
Itchy skin
If you happen to have any of these symptoms together with persistent headache or migraines and if you happen to have the risk factors for liver disease like history of alcohol abuse, NAFLD, or hepatitis, you need to get evaluated. Your doctor can help determine the cause of your headaches and whether they are related to liver disease.
How can doctors diagnose liver disease from headache symptoms?
Diagnosing liver disease and how it is related to headaches can involve a detailed approach. Your doctor will start with an extensive medical history and comprehensive physical examination. There will also be a series of tests that will be requested, including:
-
Liver function tests (LFTs)–measure the enzyme levels and protein in the blood that can indicate liver damage or inflammation.
-
Ammonia levels–if these levels are high, it may be related to hepatic encephalopathy
-
Imaging tests–ultrasound, computed tomography (CT) scan, or magnetic resonance imaging (MRI) can offer detailed images of the liver demonstrating its size, shape, and other abnormalities like tumors or scarring
-
Liver biopsy–in rare cases, small samples of liver tissue may be taken for microscopic evaluation to assess the extent and type of liver damage. This is considered the gold standard, meaning confirmatory, way of diagnosing liver disease and the exact stage.
It is important to remember that headaches are just one piece of a larger puzzle. Your healthcare provider (HCP) can consider it as part of a broader clinical picture by considering all your symptoms, medical history, and test results to arrive at an accurate diagnosis.
What Are the Treatment Options for Headaches in Liver Disease Patients?
The treatment options for headaches in liver disease always involve management of the underlying condition first. It also involves careful selection of pain relievers that are safe for an already compromised liver. The goal is to reduce the buildup of toxins and ease the symptoms without causing further liver damage.
What medications are safe for liver disease patients with headaches?

Pain relief may be a little bit complex for people with liver disease and it requires careful consideration. Here are some guidelines** to start with:
-
Low-dose acetaminophen–generally the safest over-the-counter (OTC) pain reliever available for people with liver disease, even for those with cirrhosis. When it is used in recommended low doses (not more than 2-3 grams per day), it is safe and effective. It is important that you adhere to the recommended dosage instructions given to you. Exceeding this dosage could bring harm to your liver.
-
Avoid non-steroidal anti-inflammatory drugs (NSAIDs) like naproxen, ibuprofen, and aspirin. These drugs are generally not given to patients with liver disease. These medications, while effective pain relievers, can worsen liver damage, impair kidney function, and can increase the risk of gastrointestinal bleeding. So it is not recommended to patients with liver disease, particularly those with advanced liver disease.
-
Specific treatments for HE
For headaches associated with HE, medications are often aimed to reduce ammonia levels. These include:
-
Lactulose–it is a laxative and it draws out ammonia from the blood into the colon to get excreted
-
Rifaximin–an antibiotic, which reduces the production of ammonia by bacteria in the gut
**These guidelines are meant for informational purposes only and not intended to replace professional opinion. For medical advice, consult your doctor particularly when you plan to start any medication with an ongoing liver disease.
To ensure that what you are taking is indeed safe for you, always discuss transparently with your HCP.
Are there specific treatments for hepatic encephalopathy headaches?
Yes, the most effective way to get rid of hepatic encephalopathy headaches is to treat the underlying causative factor, which is liver dysfunction. The treatment is aimed to reduce the toxins in the blood, specifically ammonia.
It is often a combination of:
-
Ammonia-reducing medications–as mentioned earlier rifaximin and lactulose are primary medications that can lower the ammonia levels. When this toxin is decreased, the neurological symptoms, including headaches, will significantly improve.
-
Dietary modifications–one of the recommendations include lowering dietary proteins but this should be done under strict medical conditions since it is required for overall health. The focus is to eat plant-based protein and ensure you are taking adequate calorie intake.
Management of the core issues surrounding liver disease could lead to resolution of the associated headaches or reduce factors that will lead to relief of hepatic encephalopathy that is responsible for many of the neurological symptoms of liver disease.
Are There Natural Remedies for Liver Disease Headaches?
Yes, there are natural remedies that are purported to be good complements for medications. However, it would be wise to consult your doctor before you start with these approaches. The primary aim for management should be to reduce factors that could worsen headaches or other neurological symptoms associated with liver disease.
Can dietary changes help reduce liver disease headaches?
Yes, dietary changes can definitely help reduce headaches associated with liver disease but not directly. Focus on eating a balanced diet, such as fruits, vegetables, and whole grains. These foods will give you the essential nutrients like vitamins, minerals, and antioxidants that will help your liver detoxification and overall health.
Foods you should consider include:
-
Berries and citrus fruits
-
Leafy vegetables and cruciferous vegetables like broccoli and cauliflower
-
Oats, brown rice, and quinoa
-
Fish, poultry, and plant-based proteins like legumes and tofu
-
Avocado, nuts, seeds, and olive oil
Conversely, here are the foods that you might want to avoid or limit since they can put additional strain on your liver and can potentially worsen liver disease.
-
Alcohol
-
High-fat foods
-
Processed foods
-
Excessive sugar and salt
What lifestyle adjustments can improve liver health and reduce headaches?
More than diet, there are several lifestyle adjustments that can make a significant difference in supporting liver function and thereby liver health. Ultimately, it leads to the reduction of liver disease-related headaches.
Some of the lifestyle changes that are recommended include:
-
Staying hydrated
-
Exercising regularly
-
Stress management
-
Quit smoking
-
Get adequate sleep and rest
-
Avoiding toxin exposure
These lifestyle changes and modifications are just supporting approaches to promote liver health and support its function when it is on the brink of impairment.
Quick Summary Box
-
Liver disease can lead to headaches, which is often due to toxin buildup like ammonia that affects brain function
-
Migraines may have a link with NAFLD, but more research is needed
-
Treatment is focused in managing the liver condition with medications like lactulose and rifaximin
-
There is a need to avoid NSAIDs
-
Natural remedies are, including liver-friendly diet, hydration, and regular exercise serve as support for liver health and potentially alleviating headaches
-
Always consult your doctor for proper diagnosis, especially if the headaches are accompanied by other neurological symptoms
Related Resources
Which Painkiller Is Safe for the Liver?
Inflamed Liver Treatment: Expert Advice on Effective Management Options
References
Ahmed, Z., Bujanda, D., & Befeler, A. (2025). Encephalopathy: Migraine Misdiagnosed: 3048 : Official journal of the American College of Gastroenterology | ACG. LWW. https://journals.lww.com/ajg/fulltext/2018/10001/encephalopathy__migraine_misdiagnosed__3048.3047.aspx
Bezerra, C. (2025, April 30). 11 Liver Disease Symptoms (Online Symptom Quiz). Tua Saúde. https://www.tuasaude.com/en/liver-disease-symptoms/
Elia, G., Luis Antonio Díaz, Eric Kauffman Ortega, Bautista, F., Eira Cerda Reyes, Martinez, S., Juan Pablo Arab, & Ramón Bataller. (2024). Alcohol-Related liver disease: A global perspective. Annals of Hepatology, 29(5), 101499–101499. https://doi.org/10.1016/j.aohep.2024.101499
Harvard Health Publishing. (2024, April 3). Acetaminophen safety: Be cautious but not afraid - Harvard Health. Harvard Health; Harvard Health. https://www.health.harvard.edu/pain/acetaminophen-safety-be-cautious-but-not-afraid
Liu, L., Daftary, M. N., Alzahrani, M. S., Ohanele, C., & Maneno, M. K. (2020). Barriers to the Treatment of Hepatitis C among Predominantly African American Patients Seeking Care in an Urban Teaching Hospital in Washington, D.C. Journal of the National Medical Association. https://doi.org/10.1016/j.jnma.2020.08.006
Mandiga, P., Foris, L. A., Kassim, G., & Bollu, P. C. (2025, January 20). Hepatic Encephalopathy. National Library of Medicine; StatPearls Publishing. https://www.ncbi.nlm.nih.gov/books/NBK430869/
Medications and the Liver - American College of Gastroenterology. (2011). American College of Gastroenterology. https://gi.org/topics/medications-and-the-liver/
Moretti, R., Caruso, P., & Gazzin, S. (2019). Non-alcoholic fatty liver disease and neurological defects. Annals of Hepatology, 18(4), 563–570. https://doi.org/10.1016/j.aohep.2019.04.007
Mukherjee, S., & John, S. (2024, February 28). Lactulose. PubMed; StatPearls Publishing. https://www.ncbi.nlm.nih.gov/books/NBK536930/
National Institute of Diabetes and Digestive and Kidney Diseases. (2019, November 27). Definition & Facts of NAFLD & NASH. National Institute of Diabetes and Digestive and Kidney Diseases. https://www.niddk.nih.gov/health-information/liver-disease/nafld-nash/definition-facts

Jaclyn P. Leyson-Azuela, RMT, MD, MPH, is a licensed General Practitioner and Public Health Expert. She currently serves as a physician in private practice, combining clinical care with her passion for preventive health and community wellness.



