Liver Damage: Causes, Signs, Symptoms, Diagnosis, and Treatment
 Written By
Blen Shumiye, MD
Written By
Blen Shumiye, MD

Your liver works tirelessly every day — filtering toxins, aiding digestion, managing hormones, and keeping your metabolism balanced. When it becomes stressed or inflamed, its ability to perform these essential tasks declines.
Liver damage happens when liver cells become injured or scarred. If untreated, it can lead to fatty liver disease, hepatitis, fibrosis, or even cirrhosis. The good news: many forms of liver damage can be slowed, managed, or even reversed with early detection and proper care.
This comprehensive guide covers early warning signs, causes, diagnosis, treatment options, and prevention strategies.
How the Liver Works
Think of your liver as your body’s natural filter and chemical factory. It:
- Removes toxins from your blood
- Stores nutrients such as iron, glucose, and vitamins
- Produces bile to help digest fats
- Manages hormones and metabolism
- Helps with blood clotting and protein production
When liver cells are damaged, these processes slow down — often causing symptoms that seem unrelated at first.
Early Warning Signs of Liver Damage

Liver disease often begins silently. However, subtle early symptoms can signal that your liver needs attention.
1. Fatigue and Low Energy
When toxins aren’t filtered properly, they stay in your bloodstream, making you feel tired or mentally foggy.
2. Loss of Appetite or Nausea
Impaired bile production can make digestion uncomfortable, especially after fatty meals.
3. Right-Sided Abdominal Pain
Inflammation or swelling can cause a dull ache under the right rib cage.
4. Yellowing of Skin or Eyes (Jaundice)
Bilirubin buildup is one of the clearest signs of liver dysfunction.
5. Dark Urine or Pale Stool
Low bile output affects the color of urine and stool.
6. Itchy Skin
Bile salts in the skin can cause persistent itching, sometimes without a rash.
7. Swelling in Legs or Abdomen
Low albumin production causes fluid buildup (edema or ascites).
8. Easy Bruising or Bleeding
A damaged liver produces fewer clotting proteins.
9. Mental Fog or Mood Changes
Toxin buildup may affect brain function, leading to confusion or irritability.
If you notice any combination of these signs, speak with a healthcare provider or try an at-home liver function test for early insights.
What Causes Liver Damage?
Liver damage stems from many sources — from lifestyle habits to genetic conditions.
1. Alcohol Misuse
Long-term drinking is a major cause of fatty liver, alcoholic hepatitis, and cirrhosis.
2. Nonalcoholic Fatty Liver Disease (NAFLD)
Common in people with:
- Overweight or obesity
- Diabetes
- High cholesterol
- Metabolic syndrome
If untreated, it can progress to NASH (a more severe inflammatory stage).
3. Viral Hepatitis (A, B, C)
- Hepatitis A: usually short-term, spread via contaminated food
- Hepatitis B & C: spread through blood or bodily fluids, can cause chronic damage
4. Medications and Toxins
Overuse or misuse of certain drugs strains the liver, including:
- Acetaminophen (Tylenol)
- Some antibiotics
- NSAIDs
- Herbal supplements like kava or comfrey
5. Autoimmune Hepatitis
The immune system mistakenly attacks liver cells. More common in women.
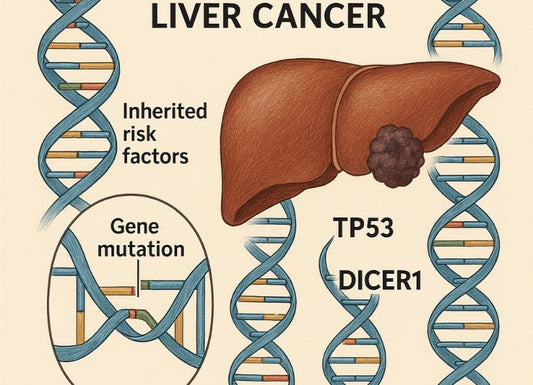
6. Genetic Disorders
- Hemochromatosis: iron overload
- Wilson’s disease: copper buildup
- Alpha-1 antitrypsin deficiency: impacts liver and lungs
7. Unhealthy Diet and Inactivity
High sugar, high fat, and low activity promote fat accumulation and inflammation.
8. Environmental Chemicals
Chronic exposure to solvents, pesticides, and industrial chemicals harms the liver.
Who Is Most at Risk?
You may have a higher risk of liver damage if you:
- Drink alcohol regularly
- Have diabetes, obesity, or metabolic syndrome
- Have high cholesterol
- Use certain medications long term
- Have viral hepatitis
- Have a family history of liver disease
- Have autoimmune or genetic conditions
Routine liver testing is especially important if you fall into these categories.
How Liver Damage Is Diagnosed

Diagnosing liver injury typically involves a combination of bloodwork, imaging, and occasionally a biopsy.
1. Blood Tests
Liver function tests (LFTs) measure:
- ALT and AST
- ALP and bilirubin
- Albumin and clotting factors
Viral, autoimmune, or genetic tests may also be performed depending on symptoms.
2. Imaging Tests
These assess liver size, shape, fat content, and scarring:
- Ultrasound
- CT or MRI
- FibroScan to measure liver stiffness (fibrosis)
3. Liver Biopsy
A small sample of liver tissue helps confirm the cause and stage of damage.
4. Genetic or Autoimmune Tests
Used when inherited or immune-related causes are suspected.
What Happens if Liver Damage Goes Untreated?
Untreated liver injury can progress into life-threatening conditions such as:
- Cirrhosis
- Liver failure
- Portal hypertension
- Ascites
- Hepatic encephalopathy
- Liver cancer (HCC)
Early detection and treatment can prevent most of these complications.
Treatment Options for Liver Damage
Treatment depends on the cause and severity. The main goal is to stop or slow progression and help the liver regenerate.
1. Addressing the Underlying Cause
- Stop alcohol immediately
- Lose weight and manage blood sugar for NAFLD
- Treat hepatitis with antiviral therapy
- Adjust medications that strain the liver
- Treat autoimmune or genetic conditions with specialized therapies
2. Medications and Supportive Therapy
Treatment may include:
- Antivirals
- Steroids or immunosuppressants
- Chelation therapy
- Vitamin or nutrient support
3. Lifestyle and Dietary Changes
Helpful habits include:
- Eating a whole-food, nutrient-rich diet
- Avoiding alcohol
- Limiting salt
- Staying hydrated
- Exercising regularly
4. Monitoring and Long-Term Care
Your doctor may recommend routine blood tests, imaging, and vaccinations for hepatitis A and B. Severe cases may require a liver transplant.
Can Liver Damage Be Reversed?
Yes — early-stage liver damage is often reversible. The liver can regenerate if:
- Alcohol is stopped
- Weight improves
- Blood sugar is controlled
- Hepatitis is treated
- Toxins are avoided
Advanced fibrosis and cirrhosis are typically permanent, but progression can still be slowed.
Preventing Liver Damage

You can protect your liver by:
- Avoiding excessive alcohol
- Maintaining a healthy weight
- Eating a whole-food diet
- Exercising regularly
- Using medications safely
- Getting vaccinated for hepatitis A and B
- Avoiding shared needles or unsterile equipment
- Getting routine tests if you’re at risk
Living Well With Liver Damage
Many people live healthy lives with mild to moderate liver disease by:
- Following medical guidance
- Avoiding alcohol
- Staying active
- Eating nutrient-dense foods
- Managing stress
When to See a Doctor
Seek medical care if you notice:
- Jaundice
- Persistent fatigue
- Unexplained weight loss
- Abdominal swelling
- Dark urine or pale stools
- Confusion or dizziness
Early evaluation is essential.
Final Thoughts
The liver is a remarkable organ with the ability to regenerate, but it’s vulnerable to viruses, toxins, metabolic stress, and autoimmune issues. Recognizing early signs such as fatigue, jaundice, or changes in urine or stool is essential for preventing long-term damage. With early testing, proper treatment, and healthy habits, most people can prevent progression and even reverse early injury.
References
American Liver Foundation. (2025). Diagnosing liver disease: Liver function tests, imaging & biopsy. https://liverfoundation.org/liver-diseases/diagnosing-liver-disease/
Cleveland Clinic. (2017, March 7). Liver Disease: Signs & Symptoms, Causes, Stages, Treatment. https://my.clevelandclinic.org/health/diseases/17179-liver-disease
Cleveland Clinic. (2023, September 6). Signs & Symptoms of Liver Failure, Causes, Treatments. https://my.clevelandclinic.org/health/diseases/17819-liver-failure
Gan, C. (2025). Liver diseases: Epidemiology, causes, trends and predictions. Signal Transduction and Targeted Therapy, 8, Article 47. https://www.nature.com/articles/s41392-024-02072-z
Liver problems – Symptoms and causes. (2025). Mayo Clinic. https://www.mayoclinic.org/diseases-conditions/liver-problems/symptoms-causes/syc-20374502
Mayo Clinic. (2025). Liver problems: Diagnosis & treatment. https://www.mayoclinic.org/diseases-conditions/liver-problems/diagnosis-treatment/drc-20374507
NHS. (2017, October). Liver disease. https://www.nhs.uk/conditions/liver-disease/
Sharma, A., & et al. (2023). Chronic liver disease: Evaluation and treatment. In StatPearls. https://www.ncbi.nlm.nih.gov/books/NBK554597/
Smith, A. (2019). Cirrhosis: Diagnosis and management. American Family Physician, 100(6), 759–768. https://www.aafp.org/pubs/afp/issues/2019/1215/p759.html
The Times of India. (2025, October 22). Liver damage warning signs visible on your hands; here’s what you need to know. https://timesofindia.indiatimes.com/life-style/health-fitness/health-news/liver-damage-warning-signs-visible-on-your-hands-heres-what-you-need-to-know/articleshow/124724908.cms
Wazir, H. (2023). Diagnosis and treatment of liver disease: Current trends. PMC, Article PMC10763979. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC10763979/

Dr. Blen is a seasoned medical writer and General Practitioner with over five years of clinical experience. She blends deep medical expertise with a gift for clear, compassionate communication to create evidence-based content that informs and empowers. Her work spans clinical research, patient education, and health journalism, establishing her as a trusted voice in both professional and public health spheres.