Liver Cirrhosis After Gallbladder Removal: Risks, Symptoms, and Prevention
 Written By
Yusela Aquino
Written By
Yusela Aquino
It’s not uncommon to feel like something’s just a little “off” after gallbladder removal—but no one really warns you about what to expect long-term. Maybe you’ve started noticing strange digestive changes, fatigue, or discomfort you didn’t have before. Or maybe a recent lab test came back with elevated liver enzymes.
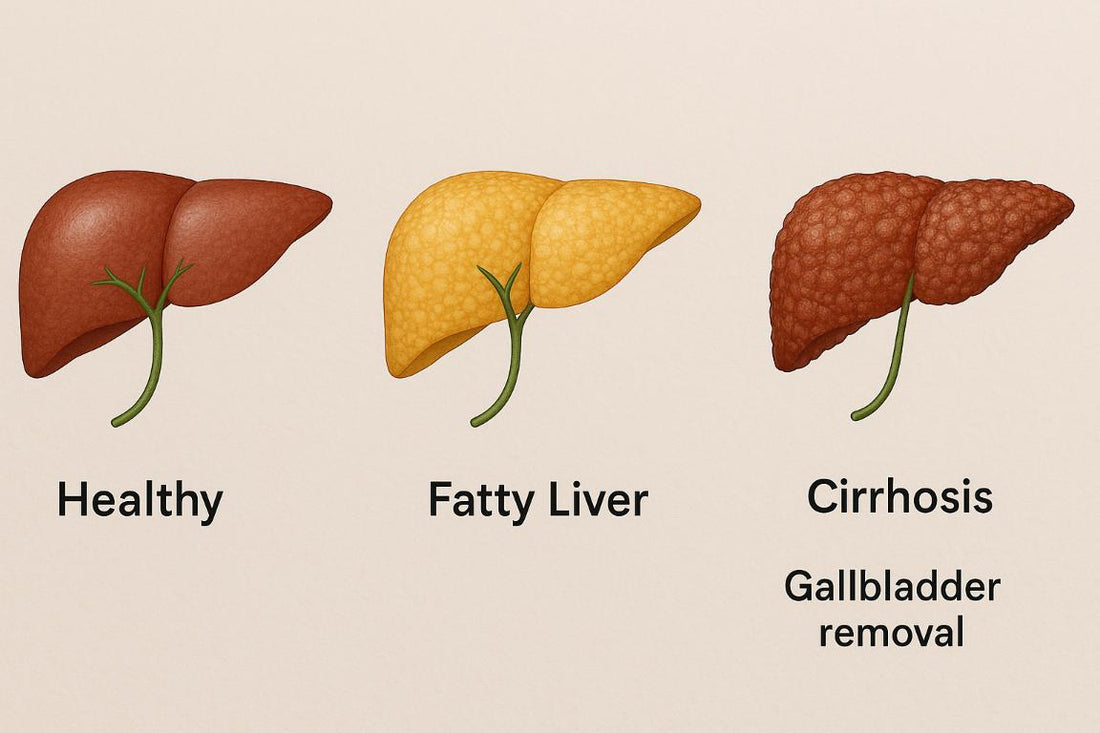
The gallbladder may not be essential for survival, but it plays an important role in how bile is stored and released. Once it’s gone, bile no longer gets released in measured bursts; instead, it trickles constantly into your digestive tract. Over time, that change in bile dynamics can throw off fat metabolism, gut health, and even your liver’s workload. In certain individuals—especially those with preexisting metabolic issues—this shift can lead to fatty liver, inflammation, and eventually fibrosis if left unchecked. The key is recognizing these changes early, and taking steps to support your liver before problems stack up.
Fatty Liver Disease Post Cholecystectomy
One of the more common liver-related issues seen after gallbladder removal is the development or worsening of fatty liver disease. Fatty liver, especially nonalcoholic fatty liver disease (NAFLD), occurs when excess fat builds up in liver cells. Without the gallbladder to regulate bile storage and release, digestion and fat metabolism can change, potentially contributing to fat accumulation in the liver.
Some studies suggest that individuals are more prone to NAFLD post-cholecystectomy, particularly if they already had metabolic syndrome, diabetes, or obesity before surgery. This makes it critical to monitor liver health in the months and years following the procedure. And good news—you can now do some of this from home with at-home liver test kits! These are super helpful for tracking your ALT, AST, and other liver enzymes.
Risk of Liver Fibrosis After Gallbladder Surgery

Liver fibrosis is a key step in the progression toward cirrhosis. It refers to the accumulation of scar tissue in the liver due to ongoing inflammation or injury. Post-cholecystectomy, bile flow becomes continuous rather than meal-triggered, and in some cases, this altered flow can contribute to chronic irritation or inflammation in the liver and bile ducts.
Patients with underlying conditions like fatty liver, hepatitis, or those with a high BMI may be particularly vulnerable. Monitoring for signs of liver fibrosis early—such as fatigue, mild abdominal discomfort, or unexpected lab changes—can help initiate timely interventions and lifestyle changes to slow or even reverse progression.
Nonalcoholic Fatty Liver Disease Following Gallbladder Removal
Nonalcoholic fatty liver disease (NAFLD) is one of the most underdiagnosed but common liver issues after gallbladder removal. NAFLD can progress to nonalcoholic steatohepatitis (NASH), which includes inflammation and may lead to fibrosis and cirrhosis. Since the gallbladder plays a role in fat digestion, its removal can alter how fats are processed, especially if dietary habits aren’t adjusted.
Post-surgical patients often find that their liver enzyme levels rise temporarily. While that might resolve on its own, it's wise to monitor them over time—especially if you experience fatigue, bloating, or upper right abdominal pain. This is where at-home liver test kits really shine—they offer a simple way to keep tabs on your liver function from the comfort of home!
Can Gallbladder Removal Cause Liver Problems?
The gallbladder and liver are closely linked, so it’s no surprise that changes in one can affect the other. While gallbladder removal is generally safe and life-saving for many, it can cause downstream effects on liver function. Most people recover without liver complications, but for some, especially those with metabolic risk factors, the liver may be more susceptible to inflammation and fat buildup.
The risk isn’t about the surgery being inherently dangerous, but rather about how the body adapts afterward. Without the gallbladder's bile storage role, the liver may become overworked, or bile flow may become erratic—potentially leading to minor or major issues. Regular follow-ups, smart lifestyle choices, and at-home test kits can make a huge difference in staying ahead of liver problems.
Post-Cholecystectomy Syndrome and Liver Complications
Post-cholecystectomy syndrome (PCS) is a term used when patients continue to experience digestive symptoms after gallbladder removal. This might include pain, bloating, indigestion, or diarrhea. Sometimes, PCS is linked to liver or bile duct issues, like bile reflux, bile duct strictures, or even early fibrosis.
When PCS is persistent, your provider might run liver function tests or imaging studies to rule out underlying liver complications. If you're experiencing vague but ongoing symptoms, don't brush them off. It's always better to get evaluated—and you can start by checking your liver enzyme levels at home!
Signs of Liver Issues After Gallbladder Removal
If you’ve had your gallbladder removed and start noticing persistent fatigue, upper abdominal pain, bloating, or jaundice (yellowing of the skin or eyes), it could be a sign of liver trouble. These symptoms should not be ignored, especially if they’re accompanied by unexplained weight changes or dark-colored urine.
Other red flags include swelling in your legs or abdomen, mental fog, or easy bruising—all of which can point to more advanced liver issues. The earlier these signs are addressed, the better your chances for a positive outcome. Regular lab tests, liver ultrasounds, or even quick at-home tests can be powerful tools in your liver care journey.
Liver Pain Following Cholecystectomy
Liver pain can be subtle or severe and may be misattributed to gastrointestinal discomfort. After gallbladder removal, some patients report a dull ache in the upper right quadrant of the abdomen, which could signal liver inflammation, bile duct irritation, or early signs of fatty liver disease.
While occasional discomfort may not mean anything serious, persistent or worsening pain warrants evaluation. A liver panel and abdominal ultrasound are usually the first steps. If you're unsure whether your pain is related to the liver, tracking symptoms and test results over time can help you and your provider pinpoint the issue.
Diagnosing Liver Cirrhosis Post Gallbladder Surgery
Diagnosing cirrhosis involves a combination of blood tests, imaging (like ultrasound), and sometimes a liver biopsy. If you've had your gallbladder removed and are experiencing symptoms suggestive of liver damage, your doctor may begin with liver function tests and look for elevated liver enzymes or abnormal bilirubin levels.
At-home liver testing kits can provide early insight and help track your levels between clinic visits. They’re not a replacement for a diagnosis, but they’re an excellent starting point for staying proactive. If cirrhosis is suspected, further diagnostic tools like elastography or MRI can assess liver stiffness and guide treatment decisions.
How to Detect Liver Damage After Gallbladder Removal
Detecting liver damage early is crucial. You don't need to wait for symptoms like jaundice or ascites to show up. Mild changes in energy, digestion, or lab values may indicate early-stage liver issues. For patients post-cholecystectomy, it’s wise to get a baseline liver panel and follow it up periodically.
Look out for trends: Are your ALT and AST slowly increasing? Is your GGT or alkaline phosphatase above normal? These subtle markers can show up before you feel anything wrong. Tracking your numbers with at-home liver tests empowers you to take action early and bring concerns to your healthcare provider promptly.
Bile Duct Injury Leading to Liver Cirrhosis
Bile duct injury is a rare but serious complication of gallbladder surgery. If the bile duct is accidentally cut or scarred during surgery, it can cause bile to leak or back up into the liver. This results in inflammation and, if left unaddressed, can lead to fibrosis and eventually cirrhosis.
Symptoms like severe pain, fever, or jaundice in the days or weeks following surgery should be urgently evaluated. Imaging like MRCP or ERCP can help diagnose a bile duct issue. If you’ve already had surgery and are feeling off, don’t wait—talk to your provider or hepatologist. Early repair and medical management can prevent long-term damage.
Metabolic Changes After Cholecystectomy and Liver Health
Cholecystectomy can influence how your body metabolizes fats and sugars. With continuous bile flow, your small intestine adapts, but sometimes not optimally. This change may shift how your liver processes nutrients, especially if you already have metabolic syndrome or prediabetes.
People may notice changes in their cholesterol levels, blood sugar stability, or weight after surgery. These shifts can increase the risk of NAFLD or worsen existing liver conditions. Lifestyle support—including personalized nutrition, exercise, and supplement strategies—can help mitigate these effects and support metabolic balance.
Long-Term Liver Risks Post Gallbladder Removal
Over the long term, patients without a gallbladder might face increased liver stress, especially if other risk factors are present. Studies show a link between gallbladder removal and the progression of NAFLD and NASH. While not everyone will develop cirrhosis, the potential is there—especially if warning signs go unchecked.
This makes it vital to stay proactive with liver-friendly habits and regular testing. Whether you check your enzyme levels every few months at your provider’s office or use an at-home liver test kit, the key is consistency. Liver damage often develops slowly, but you can catch it early with the right tools!
Diet for Fatty Liver After Gallbladder Removal
A liver-supportive diet is essential after gallbladder removal. Focus on whole foods that are high in fiber, low in saturated fats, and rich in antioxidants. Think leafy greens, cruciferous vegetables, berries, legumes, and lean proteins like fish or chicken. Incorporate omega-3s and limit simple sugars and refined carbs.
Avoid greasy, fried, and highly processed foods, which can burden your liver and digestive system. Meal timing also matters—smaller, more frequent meals can help with fat digestion. Stay hydrated and consider talking to a dietitian for a tailored plan that supports your liver health post-cholecystectomy.
Foods to Avoid with Liver Cirrhosis Post Cholecystectomy
When managing cirrhosis, especially after gallbladder removal, it’s important to avoid foods that stress the liver or worsen inflammation. High-sodium foods can cause fluid retention, while high-fat or sugar-rich foods can worsen fatty liver disease. Say no to cured meats, fast food, sugary drinks, and excessive alcohol.
Additionally, limit foods high in cholesterol and additives. Check food labels for sodium and trans fats. Patients with cirrhosis may also need to avoid raw seafood or undercooked meats due to infection risks. If you're unsure about specific foods, your provider or a liver dietitian can guide you based on your lab results and current health.
Lifestyle Changes to Prevent Liver Damage After Gallbladder Surgery

Lifestyle plays a huge role in liver health, especially post-cholecystectomy. Maintain a healthy weight, manage blood sugar levels, and stay physically active. Even light daily walks or gentle yoga can boost liver function and reduce inflammation.
Sleep, stress management, and hydration also matter. Chronic stress and poor sleep can worsen insulin resistance and increase cortisol, which impacts liver health. Make time for mental health support, joyful movement, and hydration routines. And remember—you can keep tabs on your progress with convenient at-home liver tests!
Exercise Recommendations for Liver Health Post Gallbladder Removal
Exercise can be a game-changer in protecting your liver. Aim for at least 150 minutes of moderate aerobic activity each week, like brisk walking, swimming, or cycling. Strength training two days a week can also support metabolism and reduce visceral fat, which is linked to fatty liver.
If you’re recovering from surgery or just getting started, that’s okay! Begin with low-impact movements and gradually increase intensity. Listen to your body, and celebrate small wins. Movement improves blood flow to the liver and helps regulate glucose and lipid metabolism. Pair it with healthy food choices for even better outcomes.
Managing Liver Cirrhosis After Gallbladder Surgery
If you've been diagnosed with cirrhosis after gallbladder removal, management will depend on the severity. Your doctor may recommend medications to reduce liver inflammation, treat complications, and slow progression. Lifestyle and dietary changes are also vital.
Keep up with regular blood work and imaging, and report any new symptoms promptly. Consider joining a liver health support group to stay motivated and informed. And remember—home monitoring can be a game-changer. At-home liver test kits help you track your condition between appointments and catch potential problems early.
Medications for Liver Issues Post Cholecystectomy
Medications may be prescribed depending on your liver condition. These might include vitamin supplements, bile acid binders, antifibrotic drugs, or medications to control blood sugar and cholesterol. For advanced cirrhosis, diuretics, beta blockers, or lactulose may be used.
Always talk to your doctor before starting any new medication or supplement. Some over-the-counter drugs, especially acetaminophen in high doses, can harm the liver. Keep a list of your medications and ask your provider to review them for liver safety. Monitoring liver enzyme levels at home helps ensure medications aren’t causing silent harm.
When to See a Hepatologist After Gallbladder Removal
If your liver enzymes remain elevated, if you’re experiencing persistent fatigue, unexplained weight changes, jaundice, or abdominal swelling—don’t wait. A hepatologist is a liver specialist who can dig deeper, order advanced diagnostics, and guide treatment.
Even if your symptoms are mild, getting evaluated early can help prevent more serious complications down the road. If you’re worried or unsure, listen to your gut. Book that appointment, bring your at-home liver test results, and ask every question you have. Your liver health matters!
Treatment Options for Liver Fibrosis Following Gallbladder Surgery
Treatment for liver fibrosis focuses on stopping or reversing the underlying cause. This may include treating fatty liver, managing blood sugar and cholesterol, losing weight, and avoiding alcohol. In some cases, medications that target fibrotic pathways are used under specialist guidance.
With early detection and proactive care, fibrosis can often be stabilized or even reversed. Combining a liver-supportive diet, exercise, supplements, and routine monitoring creates a powerful strategy. Tools like home testing kits make it easier than ever to stay engaged with your liver health every step of the way.
Is Fatty Liver Common After Cholecystectomy?
Yes, fatty liver is increasingly recognized as a common post-cholecystectomy issue, especially in patients with metabolic risk factors. The change in bile flow and fat metabolism can contribute to hepatic steatosis. This is particularly concerning if it progresses silently for years before symptoms emerge.
That’s why monitoring matters. Even if you feel fine, a routine liver panel or at-home test can reveal if something’s brewing beneath the surface. Knowledge is power—and in this case, it could mean the difference between mild changes and advanced disease.
In addition to finger-prick blood tests, you can now monitor your liver using a simple at-home urine test kit from Ribbon Checkup. This easy-to-use kit checks for urobilinogen and bilirubin—two key indicators of liver function and potential liver damage. Elevated levels of these markers in urine can signal early signs of liver stress, even before symptoms appear. Whether you're managing fatty liver, recovering from gallbladder surgery, or just staying proactive, Ribbon Checkup’s test gives you clear results you can trust—right from home. It's non-invasive, fast, and a valuable addition to your liver wellness toolkit.
How to Protect Liver Health After Gallbladder Removal
Protecting your liver after gallbladder removal involves a holistic approach. Eat liver-friendly foods, move your body regularly, manage stress, and avoid unnecessary medications or toxins. Get regular blood work, and if you can, use an at-home liver test to track trends and catch concerns early.
Stay curious and informed—your liver is incredibly resilient when supported! And don’t hesitate to reach out for help when needed. Your journey to optimal liver health starts with small and consistent steps!
Related Resources
- Liver Lesions: Causes, Diagnosis, and Treatment Options
- Normal Liver Size in cm by Age
- Is F3 Liver Fibrosis Reversible?
References
Chiang, D. J., Pritchard, M. T., & Nagy, L. E. (2011). Obesity, diabetes mellitus, and liver fibrosis. AJP Gastrointestinal and Liver Physiology, 300(5), G697–G702. https://doi.org/10.1152/ajpgi.00426.2010
Fallowfield, J., & Hayes, P. (2011). Pathogenesis and treatment of hepatic fibrosis: is cirrhosis reversible? Clinical Medicine, 11(2), 179–183. https://doi.org/10.7861/clinmedicine.11-2-179
Luo, D., Chen, X., Dai, Y., Kuang, F., Kang, M., Li, B., & Su, S. (2023). Cholecystectomy and risk of liver disease: a systematic review and meta-analysis of 27 million individuals. International Journal of Surgery, 109(5), 1420–1429. https://doi.org/10.1097/js9.0000000000000332
Ramalingam, G. (2023, August 5). Gallbladder Surgery in Patients with Diabetes: Managing Blood Sugar Levels - G & L Surgical. G & L Surgical. https://www.glsurgical.com.sg/gallbladder-surgery-in-patients-with-diabetes-managing-blood-sugar-levels/
Rodríguez-Antonio, I., López-Sánchez, G. N., Garrido-Camacho, V. Y., Uribe, M., Chávez-Tapia, N. C., & Nuño-Lámbarri, N. (2020). Cholecystectomy as a risk factor for non-alcoholic fatty liver disease development. HPB, 22(11), 1513–1520. https://doi.org/10.1016/j.hpb.2020.07.011
Servin-Abad, L., & Schiff, E. R. (2006, November 1). The treatment of hepatic fibrosis: reversal of the underlying disease process. https://pmc.ncbi.nlm.nih.gov/articles/PMC5368613/
Zackria, R., & Lopez, R. A. (2023, August 28). Postcholecystectomy syndrome. StatPearls - NCBI Bookshelf. https://www.ncbi.nlm.nih.gov/books/NBK539902/

Yusela is a medical student with a degree in Biology and a strong foundation in health communication. With experience in both research and clinical settings, she writes clear, evidence-informed content to help patients and caregivers better understand liver health, chronic disease, and transplant care.


