Can Liver Failure Kill You?
 Written By
Abel Tamirat, MD
Written By
Abel Tamirat, MD

Liver failure is serious. But can it kill you? The short answer is yes—especially if it’s not caught early or treated right away.
This article will explain what liver failure is, how it happens, what symptoms to watch for, and when it's considered life-threatening. We’ll also cover how treatment works, who’s most at risk, and how to improve your chances if you or someone you know is dealing with liver disease.
What is liver failure?
Liver failure means your liver is no longer working well enough to do its job. The liver filters toxins, helps with digestion, makes proteins, and balances your body’s fluids. If it fails, these vital functions break down fast.
There are two main types:
-
Acute liver failure: Happens suddenly, often within days or weeks. It can occur in someone with no history of liver disease.
-
Chronic liver failure: Happens slowly, usually after years of liver damage. It’s often caused by long-term conditions like chronic hepatitis B or C or alcohol use.
Both types are medical emergencies.
Can liver failure really be fatal?

Yes. Liver failure can absolutely be fatal. When the liver shuts down, your body quickly loses the ability to clear toxins, manage fluids, control bleeding, and support brain function.
Without treatment, these problems can spiral into:
-
Multi-organ failure
-
Brain swelling (hepatic encephalopathy)
-
Sepsis or life-threatening infections
-
Uncontrolled bleeding
-
Coma
In many cases, patients with liver failure die within days or weeks unless they receive aggressive care or a liver transplant.
How does liver failure lead to death?
Here’s what typically happens:
-
Toxins build up – The liver can’t clear waste products, especially ammonia.
-
Brain function declines – Confusion and sleepiness worsen, leading to coma.
-
Bleeding starts – The liver makes clotting factors. Without them, internal bleeding may begin.
-
Kidney failure follows – The kidneys shut down under the stress (called hepatorenal syndrome).
-
Infection risk rises – The immune system weakens, and sepsis becomes a real threat.
-
Organs fail – Without urgent care, death often follows quickly.
That’s why liver failure is considered a true emergency.
Is death always inevitable with liver failure?
No. Not all liver failure ends in death. Survival depends on:
-
The cause (e.g., acetaminophen overdose vs. cirrhosis)
-
How fast it's caught
-
Whether you get to a liver center in time
-
Your overall health
If treated early, some types of liver failure are reversible. Others may require a transplant. Some people live for years with chronic liver failure under close medical care.
Early signs to watch for
Recognizing liver failure early gives you the best chance to survive. Watch for:
-
Fatigue and weakness
-
Nausea, vomiting
-
Loss of appetite
-
Yellowing skin or eyes (jaundice)
-
Belly swelling or pain (especially upper right side)
-
Dark urine, pale stool
-
Mental fog or confusion
-
Easy bruising or bleeding
These signs mean it’s time to get checked—urgently.
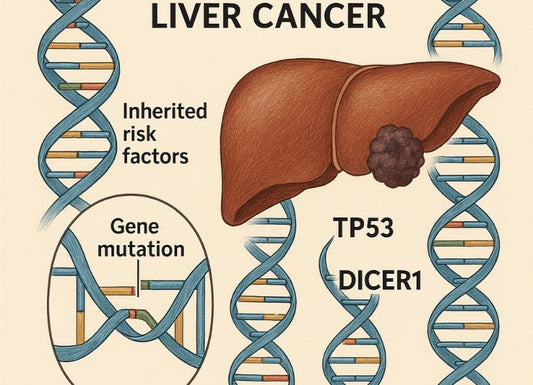
What causes liver failure?

Acute liver failure (sudden onset)
-
Viral hepatitis (especially Hep A, B, or E)
-
Drug reactions (e.g., antibiotics, anti-seizure meds)
-
Toxins (e.g., poisonous mushrooms)
-
Autoimmune hepatitis
-
Wilson’s disease (a genetic disorder)
Chronic liver failure (gradual damage)
-
Long-term alcohol use
-
Chronic hepatitis B or C
-
Fatty liver disease (NAFLD or NASH)
-
Autoimmune liver disease
-
Genetic/metabolic disorders
In both cases, if damage builds up and isn’t treated, the liver loses its ability to function—and survival is at risk.
How is liver failure treated?
Treatment depends on the cause and severity:
-
Supportive care in ICU: For hydration, nutrition, clotting support, and infection prevention
-
Medication: To manage symptoms and stop the underlying cause
-
Liver transplant: For severe or irreversible cases
Time is critical. The sooner care begins, the better the odds.
What’s the survival rate for liver failure?
It varies. But here are some general estimates:
-
Acute liver failure: Survival without a transplant ranges from 20–50%, depending on cause. With transplant, survival can be over 70%.
-
Chronic liver failure: Survival depends on how advanced the disease is. People with early cirrhosis may live for years. End-stage liver disease has a much lower survival rate.
Doctors use scoring systems like MELD (Model for End-Stage Liver Disease) to estimate risk and guide transplant timing.
When is liver failure reversible?
Some causes of acute liver failure can be reversed, especially if treated quickly. These include:
-
Acetaminophen overdose (if treated within 24 hours)
-
Autoimmune hepatitis (responds to steroids)
-
Some viral hepatitis cases
-
Drug-induced liver injury (if the drug is stopped)
In these cases, the liver may recover fully within weeks. But delay lowers the chance of reversal.
Chronic liver failure is harder to reverse. Lifestyle changes and medication can slow or stop the damage—but the liver may not heal entirely. That’s why prevention and early care matter.
What if I already have liver disease?

If you already have liver disease (like hepatitis or cirrhosis), the goal is to avoid progression to failure. You can:
-
Get regular blood tests and imaging
-
Manage your weight and blood sugar
-
Avoid alcohol and unnecessary meds
-
Get vaccinated (especially for hepatitis A and B)
-
Take prescribed medications consistently
And most importantly—stay in close contact with your liver specialist.
Can lifestyle changes prevent liver failure?
Yes, especially if caught early. Here’s what helps:
-
Avoid alcohol
-
Eat a liver-friendly diet (low salt, moderate protein, healthy fats)
-
Manage blood sugar and cholesterol
-
Exercise regularly
-
Treat viral hepatitis if diagnosed
-
Lose weight if you have fatty liver disease
Even small steps can lower your risk over time.
When should I go to the hospital?
Don’t wait if you notice:
-
Yellowing eyes or skin
-
Sudden confusion or drowsiness
-
Swollen belly
-
Vomiting blood
-
Bloody or black stool
-
Severe pain in the upper right abdomen
These are signs of advanced liver failure. Immediate care could save your life.
What about transplant?
Liver transplant is often the only cure for advanced liver failure. It replaces the damaged liver with a healthy one from a donor.
You may be a candidate if you have:
-
Acute liver failure that won’t reverse
-
Chronic liver disease with poor liver function (low MELD score)
-
Complications like ascites, encephalopathy, or bleeding
Not everyone qualifies, and wait times can be long. But transplant offers the best long-term survival in severe cases.
Takeaway
Yes, liver failure can be fatal—especially without fast medical care. But not all cases lead to death. Some are reversible, and many can be slowed or managed with treatment. A liver transplant may be life-saving if other treatments don’t work.
Know the warning signs, take early action, and follow up regularly if you have liver disease or high risk.
Worried about your liver health? Ribbon Checkup helps you track your liver health, understand your risk, and get practical guidance before problems get worse.
Related resources on Ribbon Checkup
References
Acute liver failure - Symptoms and causes. (2025). Mayo Clinic; https://www.mayoclinic.org/diseases-conditions/acute-liver-failure/symptoms-causes/syc-20352863#:~:text=Acute%20liver%20failure%20can%20develop,seek%20medical%20attention%20right%20away.
Acute Liver Failure | Conditions and Treatments | Center for Liver Disease & Transplantation | Columbia University Department of Surgery. (2024). Columbiasurgery.org. https://columbiasurgery.org/conditions-and-treatments/acute-liver-failure
and, D. (2019). Liver Disease - NIDDK. National Institute of Diabetes and Digestive and Kidney Diseases. https://www.niddk.nih.gov/health-information/liver-disease
World. (2020, March 11). Hepatitis. Who.int; World Health Organization: WHO. https://www.who.int/health-topics/hepatitis#tab=tab_1

Dr. Abel Tamirat is a licensed General Practitioner and ECFMG-certified international medical graduate with over three years of experience supporting U.S.-based telehealth and primary care practices. As a freelance medical writer and Virtual Clinical Support Specialist, he blends frontline clinical expertise with a passion for health technology and evidence-based content. He is also a contributor to Continuing Medical Education (CME) programs.