Polycystic Kidney Disease Medication: What’s Available and What’s New?
 Written By
Abel Tamirat, MD
Written By
Abel Tamirat, MD
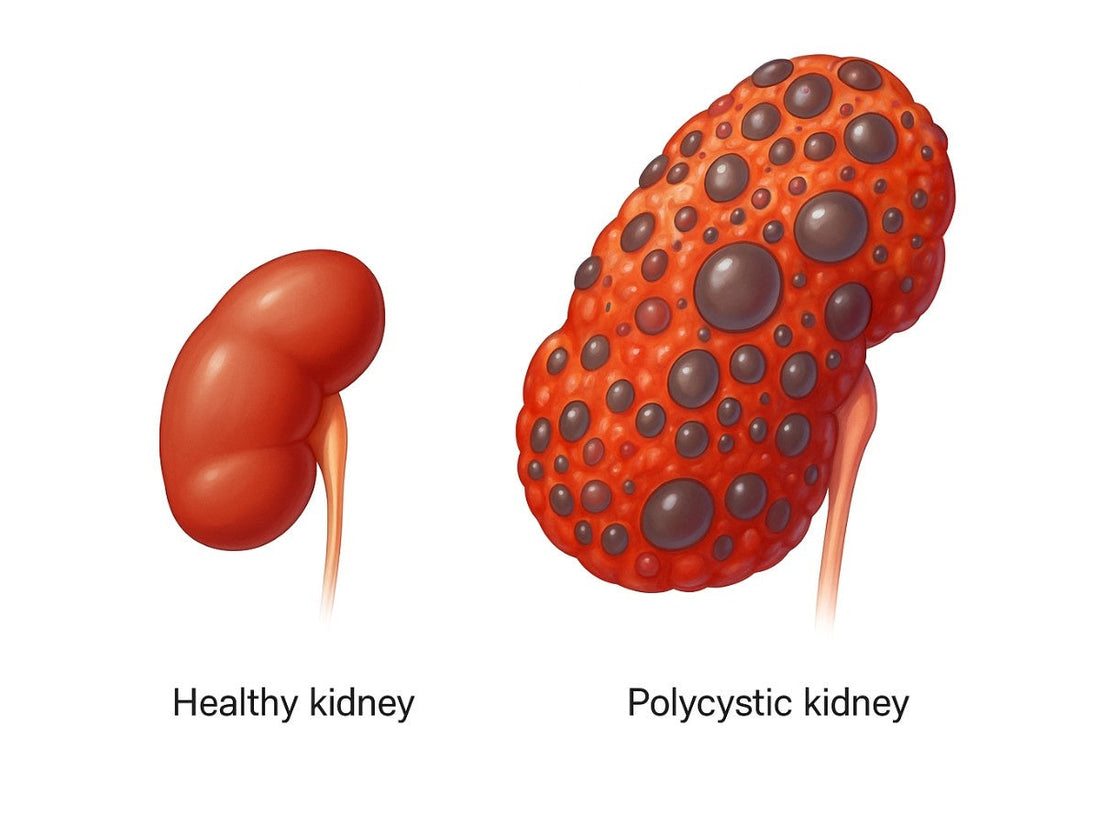
Polycystic kidney disease (PKD) affects about 600,000 people in the U.S., causing fluid-filled cysts to grow in the kidneys, which can lead to kidney failure. Medications for polycystic kidney disease are limited, but recent advances offer hope. This article explores current treatments, emerging therapies, and practical steps to manage PKD effectively.
What is polycystic kidney disease?
PKD is a genetic disorder where cysts form in the kidneys, enlarging them and impairing function over time. Autosomal dominant PKD (ADPKD) is the most common form, affecting 1 in 1,000 people, often diagnosed in your 30s or 40s. Symptoms include:
-
High blood pressure
-
Back or flank pain
-
Blood in urine (hematuria)
-
Frequent urinary tract infections
Without treatment, PKD can lead to kidney failure, requiring dialysis or a transplant. Medications aim to slow this progression and manage symptoms.
What medications are approved for PKD?

Currently, one FDA-approved drug specifically targets ADPKD, but supportive treatments also play a role.
Tolvaptan: The first approved PKD drug
Tolvaptan, approved by the FDA in 2018, is the only disease-modifying medication for adults with rapidly progressing ADPKD. It slows cyst growth by reducing the kidney’s ability to concentrate urine, which decreases fluid buildup in cysts. Studies show it can:
-
Slow total kidney volume growth by up to 50% over several years
-
Delay kidney function decline, potentially postponing dialysis by about one year per four years of treatment
How it works: Tolvaptan blocks vasopressin, a hormone that promotes cyst growth. It’s taken as an oral pill twice daily.
Side effects include:
-
Increased thirst and frequent urination
-
Nighttime urination (nocturia)
-
Potential liver toxicity (requires regular monitoring)
Tolvaptan is prescribed by nephrologists for those at high risk of progression, based on kidney size, genetics, or early symptoms. Discuss with your doctor if it’s right for you.
Supportive medications for symptoms
Other medications manage PKD symptoms, though they don’t slow cyst growth:
-
Pain relievers: Over-the-counter options like acetaminophen are often safe, but avoid NSAIDs (e.g., ibuprofen) if kidney function is impaired.
-
Blood pressure drugs: ACE inhibitors or ARBs control hypertension, which affects 50–70% of PKD patients and slows kidney damage.
-
Antibiotics: Treat urinary tract infections, common in PKD due to cysts.
Always consult your doctor before taking any medication, as some can harm kidney function. Tools like urine protein test strips and an at-home urine protein test can help monitor early damage.
What new medications are being researched?
Recent research is uncovering promising PKD treatments, focusing on slowing cyst growth and preserving kidney function.
Can glycosides help PKD?
A 2024 study found that glycosides, a class of drugs, can increase polycystin-1 levels, a protein often reduced in PKD due to gene mutations. In 3D mini-kidney models, glycosides restored polycystin function, preventing cyst formation and slowing growth in existing cysts. These drugs, originally studied for other conditions, could be tested in PKD patients soon.
Is pioglitazone a potential treatment?
Pioglitazone, an FDA-approved drug for type 2 diabetes, may inhibit chloride secretion into cysts, a key driver of cyst growth. By reducing fluid buildup, it could slow kidney enlargement. Early studies in animal models are promising, but human trials are ongoing to confirm efficacy.
What about empagliflozin?
Empagliflozin, another diabetes drug, is being studied for PKD. It belongs to the SGLT2 inhibitor class, which may reduce vasopressin activity and improve kidney function. A clinical trial at the University of Colorado is exploring its effects on ADPKD patients. Results could clarify if it slows cyst growth or delays kidney decline.

Could metformin work for PKD?
Metformin, a common diabetes drug, , has shown potential in mouse models by blocking pathways that drive cyst growth. It inhibits aerobic glycolysis, a process linked to cyst cell proliferation. Human trials are needed to validate these findings, but it’s a promising avenue.
Are gene therapies on the horizon?
Yale researchers found that a small fragment of the PKD1 gene (encoding polycystin-1) can suppress cyst growth in mice. While the full protein is too large for gene therapy, this 200-amino-acid fragment could be deliverable, opening doors to future treatments. Another study identified the Glis2 gene as a key player in PKD signaling, suggesting it as a potential therapy target. These advances are early but exciting.
Why hasn’t curcumin or niacinamide worked?
Some drugs haven’t panned out. A 2022 study at the University of Colorado found curcumin (a turmeric compound) didn’t improve kidney or vascular function in ADPKD patients. Similarly, a trial of niacinamide at the University of Kansas showed it was well-tolerated but didn’t reduce cyst growth or improve kidney function compared to placebo. These results highlight the challenge of finding effective PKD treatments.
How do medications fit into a PKD management plan?
Medications are just one part of managing PKD. A comprehensive plan includes lifestyle changes and regular monitoring.
What lifestyle changes help?
-
Stay hydrated: Drink 2.5–3 liters of water daily to suppress vasopressin, which may slow cyst growth. Discuss water intake with your nephrologist.
-
Eat a low-sodium diet: Reducing salt helps control blood pressure and protects kidney function.
-
Exercise regularly: Aim for 150 minutes of moderate activity weekly, like walking, to maintain a healthy weight.
-
Avoid smoking: Smoking worsens kidney damage and increases cyst growth risk.
You can also support kidney health with a kidney-friendly diet plan tailored to your individual condition.
How can you monitor PKD progression?
Regular checkups are crucial. Your doctor may use:
-
Blood tests: Measure kidney function (e.g., eGFR, creatinine).
-
Imaging: MRI or CT scans track total kidney volume, a predictor of progression.
-
Urine tests: Check for infections or blood in urine.
Monitoring tools such as the creatinine level guide can help you better interpret test results between doctor visits.
When should you see a doctor?

Contact your doctor if you experience:
-
Severe or persistent pain in your back or sides
-
Blood in urine or frequent infections
-
High blood pressure or headaches
-
Fever or signs of infection
-
Pregnancy complications (PKD increases pre-eclampsia risk)
If you have a family history of PKD, consult a genetic counselor for family planning.
PKD can also mimic other conditions, so knowing what can mimic kidney stone pain may help avoid misdiagnosis.
How can you stay hopeful with PKD?
Living with PKD can feel overwhelming, but advances in medications like tolvaptan and emerging therapies offer hope. Combining treatment with a healthy lifestyle and regular care can slow progression and improve quality of life.
If you’re concerned about early warning signs, explore kidney disease symptoms like nail changes that may signal deeper issues.
The Takeaway
Tolvaptan is currently the only FDA-approved medication for autosomal dominant polycystic kidney disease (ADPKD), shown to slow cyst growth and decline in kidney function. Several other medications, such as glycosides, pioglitazone, empagliflozin, and metformin, are being studied for their potential to treat PKD, though more research is needed to confirm their safety and effectiveness. In addition, gene therapy targeting PKD1 and Glis2 genes is in early development and may offer future treatment possibilities. Alongside these medical advances, lifestyle changes like maintaining healthy blood pressure, staying well-hydrated, eating a low-sodium diet, and undergoing regular monitoring remain essential parts of managing PKD.
Next step: Curious about your kidney health? Try Ribbon Checkup’s at-home kidney function test.
Related Resources
-
At-Home Urine Protein Test
Track protein levels in your urine to detect early signs of kidney damage. -
What Size of Kidney Cyst Is Dangerous?
Learn how cyst size affects kidney function and when to seek treatment. -
How to Check Kidney Function at Home
Use simple tools to monitor kidney health without visiting a clinic.
References
Ferraro, P. M., Taylor, E. N., Gambaro, G., & Curhan, G. C. (2017). Dietary and lifestyle risk factors for kidney stone formation. Urolithiasis, 45(1), 57–64. https://pubmed.ncbi.nlm.nih.gov/28281190/
Freedman, B. S., & Steinman, T. I. (2024). Glycosides as potential therapeutic agents for polycystic kidney disease. Cell Stem Cell, 31(4), 512–526. https://pubmed.ncbi.nlm.nih.gov/38599211/[](https://www.nih.gov/news-events/news-releases/scientists-discover-potential-treatment-approaches-polycystic-kidney-disease)
Khan, S. R., Pearle, M. S., Robertson, W. G., et al. (2016). Kidney stones. Nature Reviews Disease Primers, 2, 16008. https://pubmed.ncbi.nlm.nih.gov/27188687/
National Institute of Diabetes and Digestive and Kidney Diseases. (2020). Polycystic kidney disease. https://www.niddk.nih.gov/health-information/kidney-disease/polycystic-kidney-disease
Onuchic, L., & Caplan, M. J. (2023). Polycystin-1 fragment suppresses cyst growth in ADPKD mouse models. Nature Communications, 14(1), 1892. https://pubmed.ncbi.nlm.nih.gov/37031245/[](https://medicine.yale.edu/news-article/research-suggests-avenues-toward-gene-therapies-for-polycystic-kidney-disease/)
Perrone, R. D., Oberdhan, D., Ouyang, J., et al. (2023). OVERTURE: A worldwide, prospective, observational study of disease characteristics in patients with ADPKD. Kidney International Reports, 8(5), 989–1001. https://pubmed.ncbi.nlm.nih.gov/37180508/
Rehman, M., & Somlo, S. (2024). Glis2 as an effector of polycystin signaling and a target for therapy in polycystic kidney disease. Nature Communications, 15(1), 2345. https://pubmed.ncbi.nlm.nih.gov/38824123/[](https://medicine.yale.edu/news-article/polycystic-kidney-disease-treatment-gene-target-identified/)
Torres, V. E., Chapman, A. B., Devuyst, O., et al. (2018). Tolvaptan in later-stage autosomal dominant polycystic kidney disease. New England Journal of Medicine, 379(20), 1933–1942. https://pubmed.ncbi.nlm.nih.gov/30428206/[](https://pkdcure.org/about-the-disease/living-with-pkd/treatments/)
World Health Organization. (2023). Noncommunicable diseases: Kidney disease. https://www.who.int/news-room/fact-sheets/detail/noncommunicable-diseases

Dr. Abel Tamirat is a licensed General Practitioner and ECFMG-certified international medical graduate with over three years of experience supporting U.S.-based telehealth and primary care practices. As a freelance medical writer and Virtual Clinical Support Specialist, he blends frontline clinical expertise with a passion for health technology and evidence-based content. He is also a contributor to Continuing Medical Education (CME) programs.



