Nephropathy: Causes, Symptoms, Diagnosis, and Treatment
 Written By
Blen Shumiye, MD
Written By
Blen Shumiye, MD

Nephropathy is a broad term that refers to damage or disease affecting the kidneys. One specific and important type is diabetes-related kidney disease, which is a form of nephropathy caused by high blood sugar levels damaging the glomeruli and nephrons. Because the kidneys filter waste products from the blood, regulate fluid and electrolytes, and support blood pressure and hormone balance, nephropathy can lead to serious health complications if not treated promptly. Nephropathy can be detected and monitored by measuring the glomerular filtration rate, which reflects how well the kidneys are filtering blood.
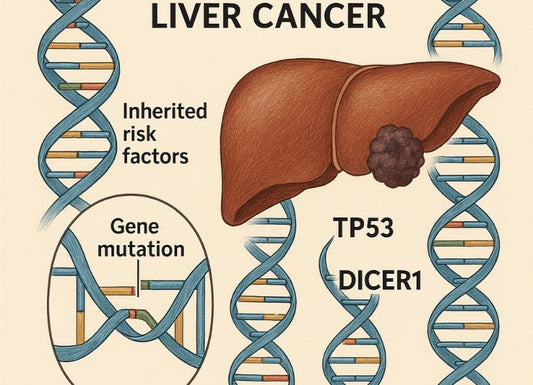
Nephropathy may be caused by diabetes, high blood pressure, autoimmune conditions, infections, toxins, or genetic disorders. Diabetes is the most common cause of nephropathy worldwide and is also the leading cause of end-stage renal disease (ESRD). Early diagnosis and treatment can significantly slow or prevent kidney damage.
This guide explains the types of nephropathy, warning signs, treatment options, and steps to protect your kidney health.
What Is Nephropathy?
Nephropathy means kidney disease or kidney damage. It can involve:
-
The glomeruli (filtering units that are part of the kidney’s filtering system)
-
The tubules (small tubes that process fluid and waste)
-
The blood vessels of the kidneys
-
The interstitial tissue between kidney structures
-
The renal parenchyma, which is the functional tissue of the kidney responsible for filtration and waste removal
The kidneys contain millions of tiny blood vessel clusters called glomeruli that filter waste from the blood, playing a critical role in maintaining overall health.
Blood flows through the kidney’s network of capillaries, supporting the filtering system by allowing waste removal and fluid regulation.
Common forms of nephropathy include diabetic nephropathy, hypertensive nephropathy, and glomerulonephritis.
Types of Nephropathy
1. Diabetic Nephropathy (Most Common)
Long-term high blood sugar, especially in people with type 2 diabetes, damages the tiny blood vessels of the kidneys and is a leading cause of diabetic nephropathy.
Key features:
-
Protein called albumin in the urine
-
Microalbuminuria (small amounts of albumin in the urine) is often the earliest detectable sign of diabetic nephropathy
-
Gradual loss of kidney function
-
Often progresses silently
Having small amounts of protein in the urine is called microalbuminuria, while larger amounts are referred to as macroalbuminuria.
Diabetic nephropathy affects the kidneys by damaging their filtering system, which leads to decreased kidney function and can result in kidney failure or end-stage kidney disease.
2. Hypertensive Nephropathy
Chronic high blood pressure injures kidney vessels and reduces filtration. This process can lead to arteriolar nephrosclerosis, which is the thickening and hardening of the small arteries in the kidneys.
3. Glomerular Nephropathy (Glomerulonephritis)
Inflammation of the kidney’s filtering units.
Causes include:
-
Autoimmune diseases (lupus, IgA nephropathy)
-
Immune complex deposition in the glomeruli is a common underlying mechanism in many types of glomerulonephritis.
-
-
Infections
-
Vasculitis
4. Drug-Induced Nephropathy
Certain medications or toxins can damage the kidneys. Nephrotoxic drugs, such as certain pain medicines and antibiotics, can cause drug-induced nephropathy.
Examples:
-
Pain medicines such as NSAIDs (ibuprofen, naproxen)
-
Certain antibiotics
-
Contrast dyes
5. Obstructive Nephropathy
Blockages such as kidney stones or enlarged prostate can harm the kidneys. These blockages can cause hydronephrosis, which is the swelling of the kidney due to a buildup of urine.
6. Hereditary Nephropathy
Genetic disorders like polycystic kidney disease cause cysts or structural changes.
Alport syndrome is another hereditary nephropathy, characterized by progressive kidney disease, hearing loss, and eye abnormalities.
Early Symptoms of Nephropathy

Many people have no symptoms in the early stages. As kidney function declines, signs may include:
-
Swelling in the legs, ankles, or around the eyes (edema)
-
Foamy or bubbly urine
-
Frequent urination (especially at night)
-
Fatigue or weakness
-
High blood pressure
-
Nausea or reduced appetite
A urine test can help detect early signs of nephropathy, such as protein (albumin) in the urine.
Symptoms often appear only when kidney damage becomes advanced.
Advanced Symptoms
These symptoms typically appear in the later stages of nephropathy.
As nephropathy progresses, more serious symptoms may develop:
-
Shortness of breath
-
Severe swelling
-
Difficulty concentrating
-
Muscle cramps
-
Itching
-
Darkening of skin
-
Severe fatigue
These symptoms may be signs of uremia, a condition where waste products build up in the blood due to severe kidney dysfunction.
These indicate significant kidney dysfunction.
In the final stage of nephropathy, kidney function may be completely lost, requiring dialysis or transplantation. This stage is known as end-stage renal disease (ESRD).
Causes and Risk Factors
Kidney disease can be triggered by a variety of medical conditions.
Major risk factors include:
-
Diabetes (leading cause)
-
High blood pressure
-
Heart disease
-
Autoimmune disorders (such as systemic lupus erythematosus)
-
Family history of kidney disease
-
Kidney infections
-
Frequent use of NSAIDs
-
Obesity
-
Smoking
Nephropathy can also increase the risk of other complications related to diabetes and kidney disease.
How Nephropathy Is Diagnosed

Diagnosis typically involves blood tests, urine tests (which may check for red blood cells and how much protein is present), imaging such as renal ultrasound, and sometimes a biopsy.
1. Blood Tests
-
eGFR to estimate kidney function (To learn more, see Creatinine level for Stage 3 Kidney)
-
Creatinine levels
-
Serum creatinine
-
BUN (blood urea nitrogen)
2. Urine Tests
-
Urine albumin-to-creatinine ratio
-
Protein or blood in the urine (hematuria)
3. Imaging Tests
-
Ultrasound
-
CT scan (if needed)
-
CT urography (for detailed imaging of the urinary tract)
4. Kidney Biopsy
Used for unclear or suspected autoimmune causes.
Kidney biopsy samples are typically examined using light microscopy to identify patterns of kidney injury.
Complications of Nephropathy
Without treatment, nephropathy may lead to:
-
High blood pressure
-
Fluid retention
-
Electrolyte imbalance
-
Metabolic acidosis
-
Anemia
-
Bone disease
-
Kidney failure, including progression to end stage kidney disease (ESKD), which may require dialysis or a kidney transplant as treatment options.
Prognosis of Nephropathy
Your outlook depends on the cause of kidney disease, how early it’s detected, and how well it’s managed. Key points:
-
Managing diabetic nephropathy:
-
Maintain a healthy weight
-
Stay active
-
Follow a balanced diet
-
Work closely with your healthcare provider or kidney specialist
-
-
Risks of untreated kidney disease:
-
Faster progression to kidney failure
-
Increased risk of heart disease
-
Possible need for dialysis or a kidney transplant
-
-
Benefits of early detection and treatment:
-
Regular urine tests and blood sugar monitoring
-
Medications such as ACE inhibitors to lower blood pressure and protect kidney function
-
Many people can slow disease progression with consistent care
-
-
Support and lifestyle:
-
Support groups and education help with motivation and informed decision-making
-
Healthy habits and coordinated medical care improve overall health and quality of life
-
Self-Care and Lifestyle Changes for Nephropathy
If you're living with diabetic nephropathy—or any form of kidney disease—you can take meaningful steps to protect your health every single day. Your medical treatments are essential, but the choices you make daily can truly help slow kidney disease progression.
You have more control than you might think. Here are caring, evidence-based strategies to help protect your kidneys and support your overall well-being:
-
Adopt a Kidney-Friendly Diet
-
Stay Physically Active
-
Stay Hydrated
-
Avoid Smoking and Limit Alcohol
-
Manage Stress
-
Monitor Your Health Regularly
-
Take Medications as Prescribed
-
Seek Support.
You can make a real difference in slowing diabetic nephropathy progression and improving your quality of life. Even small changes add up to meaningful benefits over time.
Remember, you're not walking this path alone. Working closely with your healthcare team ensures you have the guidance and support you need every step of the way.
Treatment for Nephropathy
Treatment depends on the cause but often includes medication—taking medications as prescribed is crucial—lifestyle changes, and monitoring. Using medications and lifestyle changes to lower blood pressure is a key component of nephropathy treatment, as it helps preserve kidney function and slow disease progression. Medication to lower blood pressure is particularly important in managing diabetic nephropathy.
A nephrology referral may be necessary for patients with advanced or rapidly progressing nephropathy.
1. Blood Sugar Control (For Diabetic Nephropathy)
Better control of blood glucose levels slows kidney damage. Maintaining optimal glycemic control is essential for preventing the progression of diabetic nephropathy.
Helpful medications:
-
SGLT2 inhibitors
-
GLP-1 medications
-
Insulin
2. Blood Pressure Management
Target: below 130/80 mmHg.
Medications:
-
ACE inhibitors
-
ARBs (angiotensin receptor blockers)
3. Reducing Protein in Urine
ACE inhibitors and ARBs lower albuminuria. Reducing proteinuria is a key goal in the management of nephropathy.
4. Avoiding Kidney-Damaging Medications
Limit NSAIDs and discuss alternatives with your doctor.
5. Managing Underlying Conditions
-
Treat autoimmune disease with immunosuppressants (such as lupus nephritis)
-
Remove obstructions like stones
-
Treat infections promptly
6. Diet and Lifestyle Changes
-
Follow a healthy diet
-
Low-sodium diet (sodium restriction)
-
Moderate protein intake
-
Control blood sugar and cholesterol
-
Maintain a healthy weight
-
Avoid smoking
7. Regular Monitoring
Kidney function tests every 3 to 6 months, depending on severity. Regular albuminuria monitoring is also important for tracking disease progression.
Can Nephropathy Be Reversed?
Some forms can improve, especially when treated early.
Reversible cases include:
-
Nephropathy from dehydration
-
Medication-related nephropathy
-
Obstructive nephropathy (after blockage removal)
-
Acute interstitial nephritis
Chronic nephropathy from diabetes or hypertension is usually not reversible, but progression can be slowed or stabilized for years.
When to See a Doctor

Seek medical evaluation if you notice:
-
Foamy urine
-
Persistent swelling
-
Rising blood pressure
-
Frequent urination at night
-
Family history of kidney disease
If you have persistent or worsening symptoms, you should consult a nephrologist for specialized care.
Seek urgent care for:
-
Severe abdominal or back pain
-
Sudden decrease in urine output
-
Shortness of breath
Research and Developments in Nephropathy
Ongoing research in diabetic nephropathy is improving how we understand, detect, and treat diabetic kidney disease. Scientists now better understand how high blood sugar damages kidney blood vessels, leading to progressive disease or, in severe cases, kidney failure.
New medications offer added protection for kidney function. ACE inhibitors remain a key treatment for lowering blood pressure and reducing urine protein, while newer drugs like GLP-1 receptor agonists show promise for both blood sugar control and kidney support.
Diagnostic tools are also advancing. Kidney biopsies still help identify early disease, and emerging urine tests can detect biomarkers of early kidney injury. Regular monitoring of creatinine and urine protein helps track how well your kidneys are working.
Lifestyle measures continue to play a major role. Maintaining a healthy weight, eating well, staying active, and participating in support or education programs can reduce your risk and slow disease progression.
Working closely with your healthcare team including a kidney specialist when needed remains essential. With ongoing research and improved treatment options, the outlook for preventing and managing diabetic kidney disease is steadily improving.
The Bottom Line
Nephropathy refers to kidney damage from various causes, including diabetes, hypertension, autoimmune disorders, and toxins. Renal impairment can result from any of these causes and may progress if not managed appropriately. Early stages often have no symptoms, making regular testing essential for prevention and early intervention.
With proper treatment — including blood sugar and blood pressure control, medication, lifestyle changes, and regular monitoring — many people can slow or stop the progression of nephropathy and protect kidney health.
Want to check your kidney function from home?
You can take an at-home kidney and metabolic panel test through Ribbon Checkup and get results in days.
Related sources
-
Can Kidney Disease Cause Weight Gain? Insights on Connection
-
7-Day Meal Plan For Kidney Disease and Diabetes—Supporting Your Kidneys
References
Chronic Kidney Disease (CKD). (2025, November 27). National Kidney Foundation. https://www.kidney.org/kidney-topics/chronic-kidney-disease-ckd
Diabetes-Related Nephropathy: Causes, Symptoms & Treatment. (2022, September 21). Cleveland Clinic. https://my.clevelandclinic.org/health/diseases/24183-diabetic-nephropathy
Diabetic nephropathy (kidney disease) - Symptoms and causes. (2025). Mayo Clinic; https://www.mayoclinic.org/diseases-conditions/diabetic-nephropathy/symptoms-causes/syc-20354556
Karstina, M. (2024). Understanding Nephropathy: Causes, Symptoms and Treatment. Journal of Nephrology & Therapeutics, 14(3), 1–2. https://doi.org/10.37421/2161-0959.2024.14.509
Vaidya, S. R., & Aeddula, N. R. (2024, July 31). Chronic Kidney Disease. Nih.gov; StatPearls Publishing. https://www.ncbi.nlm.nih.gov/books/NBK535404/

Dr. Blen is a seasoned medical writer and General Practitioner with over five years of clinical experience. She blends deep medical expertise with a gift for clear, compassionate communication to create evidence-based content that informs and empowers. Her work spans clinical research, patient education, and health journalism, establishing her as a trusted voice in both professional and public health spheres.