Horseshoe Kidney: What It Means for Your Health
 Written By
Blen Shumiye, MD
Written By
Blen Shumiye, MD
Your kidneys are two bean-shaped organs that filter waste, balance fluids, and regulate vital functions. They filter waste, balance fluids, regulate blood pressure, and support red blood cell production. But not every kidney forms in the same way. One of the most common congenital (present at birth) differences is called horseshoe kidney, where the two kidneys fuse together at their lower ends, creating a U-shape.
For some people, this unusual shape never causes trouble. They may go their whole lives without even realizing they have it. For others, it can raise the risk of urinary tract infections, kidney stones, or other complications that affect overall health.
If you or your child has been diagnosed with a horseshoe kidney, it’s natural to feel uncertain. You may be asking: What caused this? Will it affect kidney function? Is treatment necessary? This guide answers those questions in plain language, helping you understand causes, symptoms, diagnosis, treatment options, and what horseshoe kidney means for your long-term health.
What Is a Horseshoe Kidney?
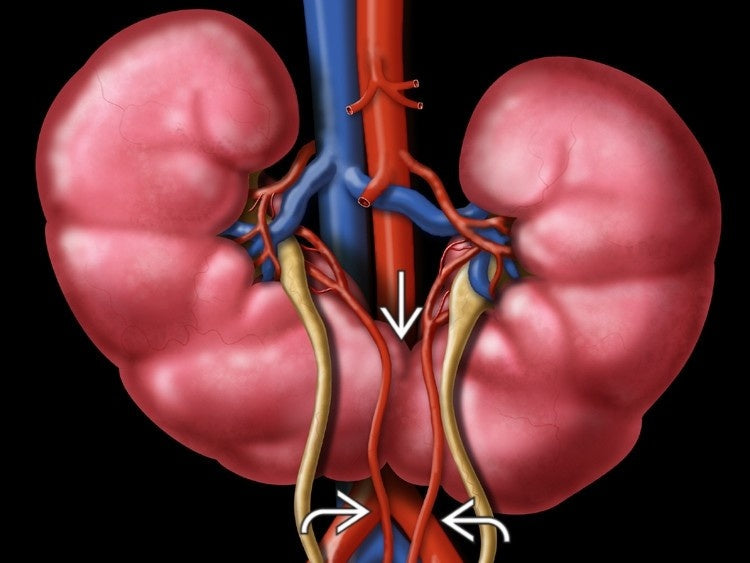
Normally, kidneys develop separately on each side of the spine. In horseshoe kidney, however, the lower ends of the two kidneys fuse together before birth. This creates a U-shaped organ that sits lower in the abdomen than usual.
Horseshoe kidney is rare, affecting about 1 in 500 people. It’s more common in men than in women and is often discovered accidentally during imaging tests for unrelated reasons.
The fusion doesn’t always interfere with kidney function. Many people live normal lives without ever experiencing symptoms. But the altered structure and location of the kidneys can sometimes lead to health issues, particularly involving the urinary tract.
What causes a horseshoe kidney?
Horseshoe kidney develops before birth, while the baby is still in the womb. Normally, the kidneys form low in the pelvis and move upward as the fetus grows. In horseshoe kidney, the lower ends fuse together before this migration is complete.
This fusion creates a tissue band called the isthmus, which keeps the kidneys joined. While not dangerous by itself, the isthmus can affect how the kidneys sit in the body and how nearby blood vessels and ureters (urine tubes) function.
Researchers don’t know the exact cause, but both genetic and developmental factors are believed to play a role. Sometimes horseshoe kidney appears with conditions like:
-
Trisomy 18 (Edwards syndrome)
-
Trisomy 13 (Patau syndrome)
-
Other urinary tract differences
Still, many people with horseshoe kidney are otherwise completely healthy.
Symptoms of Horseshoe Kidney

Not everyone with horseshoe kidney experiences symptoms. In fact, many people only discover they have it when an imaging scan is done for another reason. But when symptoms do occur, they are usually linked to complications caused by the kidney’s unusual position or structure.
Common Symptoms and Complications
-
Urinary tract infections (UTIs): The altered shape can make it harder for urine to drain properly, increasing infection risk. Symptoms may include pain or burning during urination, frequent urination, or cloudy urine. Home urinary tract infection test strips can help detect early infections.
-
Kidney stones: Because urine flow may be slower, minerals can build up and form stones. This can lead to severe flank pain, nausea, or blood in the urine.
-
Hydronephrosis: When urine backs up into the kidneys due to obstruction, they can become swollen and painful.
-
Abdominal or flank pain: Some people feel a dull ache or discomfort in the lower back or sides.
-
Digestive symptoms: Because the fused kidneys sit lower than normal, they may sometimes press on the intestines, causing bloating, nausea, or stomach discomfort.
-
High blood pressure (hypertension): In some cases, abnormal blood vessel connections associated with horseshoe kidney can contribute to elevated blood pressure.
Monitoring kidney function with at-home kidney function tests can help catch early issues.
Diagnosis of Horseshoe Kidney

Because horseshoe kidney often doesn’t cause noticeable symptoms, many people discover it only after undergoing an imaging test for another reason, such as abdominal pain or kidney stones.
Common Diagnostic Tools
-
Ultrasound: A noninvasive test that uses sound waves to visualize the kidneys.
-
CT scan or MRI: Provides detailed images of the kidneys, ureters, and surrounding structures.
-
IVP (intravenous pyelogram): A type of X-ray that tracks dye as it moves through the urinary system.
-
Voiding cystourethrogram (VCUG): Especially in children, this test can help identify reflux (when urine flows backward from the bladder to the kidneys).
These tests confirm the presence of the fused kidneys and help doctors check for blockages, stones, or other issues.
Understanding normal kidney size can help interpret imaging results.
Treatment Options for Horseshoe Kidney
Not every case of horseshoe kidney needs treatment. If you don’t have symptoms and your kidney function is normal, doctors may simply monitor your condition.
When Treatment Is Needed
Treatment focuses on managing complications rather than “fixing” the horseshoe kidney itself, since the fusion cannot be reversed. Common treatments include:
-
Urinary tract infections (UTIs): Antibiotics are used to clear infections. Preventive strategies such as staying hydrated and practicing good bathroom habits may also help.
-
Kidney stones: Treatment depends on the size and location of the stone. Options may include pain management, medications, shock wave lithotripsy (breaking stones into smaller pieces), or surgery if the stones are large or recurrent.
-
Hydronephrosis or blockages: Surgery may be required to remove obstructions and restore proper urine flow.
-
Pain management: Some people may need medications or minimally invasive procedures if pain persists.
-
High blood pressure: If linked to blood vessel abnormalities, medications or surgical correction may be needed.
Living With Horseshoe Kidney

Most people with horseshoe kidney live normal, healthy lives, especially if the condition is discovered early and monitored appropriately. Still, it’s important to take certain precautions and prioritize kidney health.
Lifestyle Tips
-
Stay hydrated: Drinking enough water helps flush bacteria and reduce the risk of stones.
-
Eat a balanced diet: Limiting excess salt, processed foods, and too much animal protein can support kidney health.
-
Avoid smoking and heavy drinking: Both increase the risk of kidney and urinary tract complications.
-
Protect your abdomen: Because horseshoe kidneys sit lower, they may be more vulnerable to injury from accidents or sports impacts. Wearing protective gear may help.
-
Schedule regular check-ups: Imaging tests and urine or blood work can help monitor kidney function over time.
Children With Horseshoe Kidney
For children, horseshoe kidney is often discovered during prenatal or early childhood ultrasounds. While some children may face higher risks of UTIs or reflux, many grow up healthy with proper monitoring and treatment. Parents should work closely with pediatric nephrologists or urologists to ensure their child’s kidneys are functioning well.
Long-Term Outlook
The outlook for people with horseshoe kidney is generally good. The condition itself doesn’t shorten life expectancy, and many people remain symptom-free. However, the risk of complications means regular monitoring is important.
Horseshoe kidney has been linked to a slightly higher risk of certain kidney cancers, but the overall risk remains low. Most people never experience serious health problems directly because of the condition.
The key is awareness: knowing you have horseshoe kidney allows you and your doctor to be proactive about monitoring and managing your kidney health.
When to See a Doctor
Seek medical advice if you experience:
-
Persistent back, side, or abdominal pain
-
Frequent urinary tract infections
-
Blood in your urine
-
Trouble urinating or decreased urine output
-
High blood pressure that is difficult to control
Catching and addressing complications early can prevent long-term kidney damage.
Conclusion
Horseshoe kidney is one of the most common congenital kidney differences, yet many people never know they have it. For most, it doesn’t interfere with daily life or kidney function. But for some, it can increase the risk of UTIs, kidney stones, and other complications.
The good news is that with monitoring, lifestyle adjustments, and treatment when necessary, people with horseshoe kidney can live long, healthy lives. If you or your child has been diagnosed, stay informed, maintain regular check-ups, and work with your healthcare provider to protect kidney health for the future.
Concerned about your kidney health?
Ribbon Checkup helps you monitor your kidney function from home, detect potential complications early, and take proactive steps to protect your long-term health. Don’t wait for symptoms to appear early screening makes all the difference.
Related sources
References
Cassell, A., Jalloh, M., Diop, P. S., Mbodji, M. M., Ndoye, M., Diallo, A., Saint Charles Kouka, Issa Labou, Niang, L., & Gueye, S. M. (2020). A Review of Rare Associations of Horseshoe Kidney: Highlight of a Rare Clinical Case of Polycystic Horseshoe Kidney, Liver Cyst, and Uterine Prolapse. EMJ Urology. https://doi.org/10.33590/emjurol/19-00185
Horseshoe Kidney (Renal Fusion): Causes & Treatment. (2021, September 10). Cleveland Clinic. https://my.clevelandclinic.org/health/diseases/21745-horseshoe-kidney-renal-fusion?utm_source=chatgpt.com
Kumar, G., Stern, J., & Leslie, S. W. (2025, September 14). Horseshoe Kidney. Nih.gov; StatPearls Publishing. https://www.ncbi.nlm.nih.gov/books/NBK431105/?utm_source=chatgpt.com
Taghavi, K., Kirkpatrick, J., & S.A. Mirjalili. (2016). The horseshoe kidney: Surgical anatomy and embryology. Journal of Pediatric Urology, 12(5), 275–280. https://doi.org/10.1016/j.jpurol.2016.04.033

Dr. Blen is a seasoned medical writer and General Practitioner with over five years of clinical experience. She blends deep medical expertise with a gift for clear, compassionate communication to create evidence-based content that informs and empowers. Her work spans clinical research, patient education, and health journalism, establishing her as a trusted voice in both professional and public health spheres.



