Alcohol and Your Kidneys: Early Signs of Damage to Watch For
 Written By
Abel Tamirat, MD
Written By
Abel Tamirat, MD
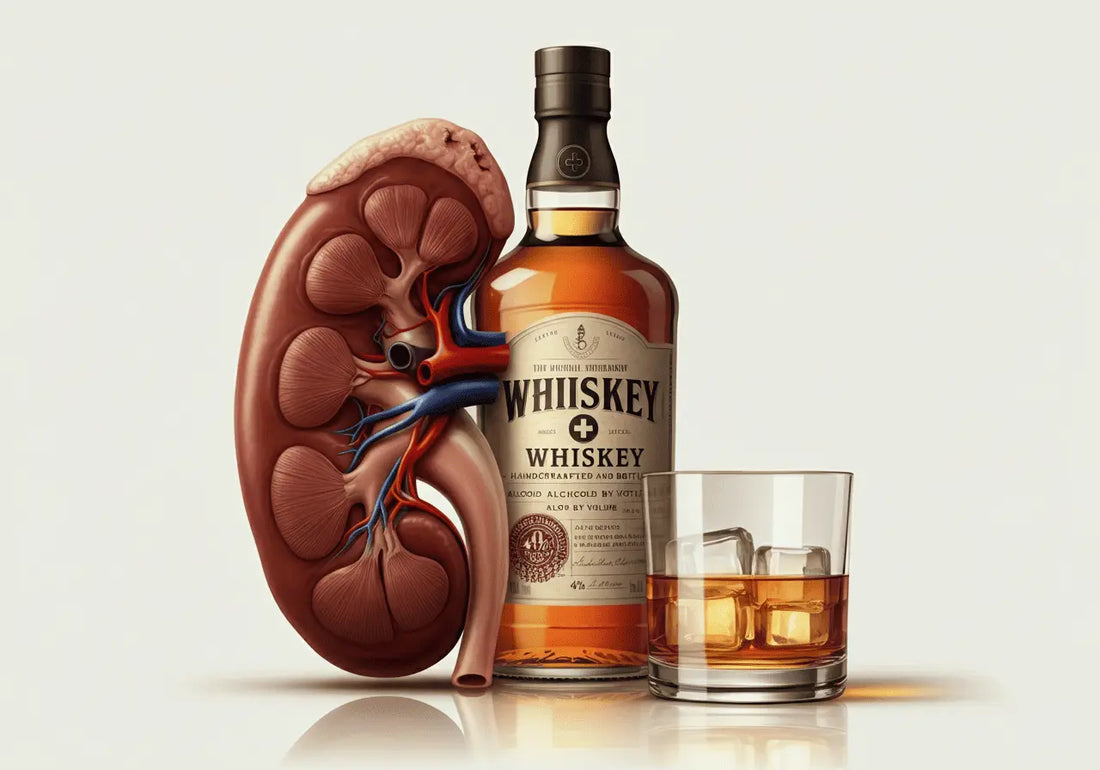
You may already know that heavy drinking can damage your liver, but what about your kidneys?
These bean-shaped organs are the body’s natural filtration system, working 24/7 to eliminate toxins, balance electrolytes, and regulate blood pressure. Yet alcohol, especially when consumed heavily or frequently, can silently sabotage these vital functions.
According to the National Kidney Foundation, 1 in 7 adults in the U.S. has chronic kidney disease (CKD), and many don’t know it. Could alcohol be playing a role in that silent epidemic?
This guide unpacks the science behind alcohol-related kidney damage, helps you recognize early warning signs, and outlines proactive steps to protect your long-term health.
How Alcohol Affects Kidney Function
Your Kidneys: The Body’s Detox Pros
Kidneys filter roughly 50 gallons of blood every single day. They remove waste, regulate blood pressure, maintain fluid balance, and manage electrolytes like sodium and potassium. But when alcohol enters the equation, everything shifts.
What Alcohol Does
-
Dehydrates you: Alcohol blocks the release of vasopressin, a hormone that tells your kidneys to retain water. The result? More urine, less fluid, and greater strain.
-
Diverts kidney function: Because your body prioritizes clearing alcohol as a toxin, your kidneys put other essential tasks on hold.
-
Disrupts mineral balance: The fluid loss can lead to electrolyte imbalances that impair heart, nerve, and muscle function.
Repeated over time, this strain can cause inflammation and oxidative stress inside your kidneys—damaging the nephrons, the tiny filtering units inside each kidney. You can monitor this damage early by using urine protein test strips to check for elevated protein levels.
What Happens After a Few Drinks
Even a casual night of drinking can trigger temporary kidney stress:
-
Increased urination: You lose more fluids than you consume, especially without water.
-
Mild dehydration: Headaches, fatigue, and lightheadedness are signs your kidneys are straining to maintain fluid balance. In fact, studies show that even temporary dehydration from alcohol can increase the workload on kidneys significantly.
-
Blood pressure swings: Alcohol may lower your pressure while drinking, but causes rebounds that elevate it hours later.
While these effects usually pass, the damage adds up. Think of it as repeatedly running your engine on low oil—eventually, something gives.
How Alcohol Promotes Chronic Kidney Disease

The danger isn’t always in the hangover. Over months or years, alcohol can cause long-lasting harm.
What Chronic Use Leads To
-
Chronic Kidney Disease (CKD): The gradual, often silent loss of kidney function.
-
Nephron damage: Inflammation and scarring inside filtering units make waste removal harder.
-
Hypertension (high blood pressure): A leading cause—and consequence—of kidney dysfunction.
-
Liver disease complications: Reduced liver function means kidneys must take on more toxic load.
Even non-daily drinking can be risky. Binge drinking—4+ drinks for women or 5+ for men in about 2 hours—can trigger acute kidney injury (AKI), a sudden loss of kidney function. Though rare, AKI can result from dehydration, low blood pressure, or muscle breakdown, and in severe cases, may require dialysis.
Acute kidney injury often goes unnoticed but is a critical warning sign of worsening kidney function.
How High Blood Pressure Makes It Worse
Your kidneys help control blood pressure by managing fluid levels and producing hormones. But alcohol disrupts this balance:
-
It causes blood vessels to narrow.
-
It raises your heart rate.
-
It interferes with hormones that regulate pressure.
This can result in chronic high blood pressure, which damages kidney blood vessels. For people who already have hypertension, alcohol accelerates kidney decline.
If you're already hypertensive, it's essential to understand how creatinine levels reflect the impact of both alcohol and blood pressure on kidney performance.
How Liver Damage Makes Things Worse for Kidneys
The liver and kidneys are teammates in detoxing your body. But alcohol puts them both at risk.
How Liver Disease Affects Kidneys
-
Reduced blood flow: A cirrhotic liver restricts the blood supply to kidneys.
-
Toxin overflow: A compromised liver means kidneys must handle more impurities.
-
Hepatorenal syndrome: In severe liver failure, kidney function can rapidly collapse.
Even before cirrhosis, fatty liver or fibrosis increases kidney workload. If you’ve been told you have liver issues, protecting your kidneys should be part of the plan.
Learn more about early detection of liver disease and how it’s tightly linked to kidney strain due to toxin overload.
Early Signs of Kidney Damage from Alcohol

Kidneys don’t usually scream for help until late-stage disease. But your body may give subtle signals. Look out for:
-
Changes in urination: More or less frequent, foamy, or reddish urine
-
Swelling: Especially in feet, ankles, hands, or under the eyes
-
Fatigue or brain fog: Even after restful sleep
-
Persistent lower back pain: Around the kidneys
-
Dry, itchy skin or nighttime muscle cramps
-
Nausea, vomiting, or appetite loss
-
Difficulty concentrating or trouble sleeping
Noticing several symptoms together? Ask your doctor about a kidney panel and urinalysis.
Alcohol also can worsen protein in urine, which is one of the earliest measurable signs of kidney filtration issues.
Alcohol-Related Kidney Conditions
Excessive alcohol consumption is linked to multiple kidney conditions:
-
Chronic kidney disease (CKD): Long-term decline in kidney function
-
Acute kidney injury (AKI): Sudden kidney failure, often due to binge drinking
-
Glomerulonephritis: Inflammation of kidney filtering structures
-
Alcoholic nephropathy: A general term for alcohol-related kidney damage
If untreated, these conditions can progress to End-Stage Renal Disease (ESRD), requiring dialysis or transplant.
Alcohol, Diabetes, and Kidney Health
Alcohol and diabetes don’t mix well—especially when it comes to kidney health. Drinking can make it harder to control your blood sugar levels, which increases your risk of diabetic kidney disease.
If you already have diabetes, alcohol can interfere with insulin sensitivity and cause dangerous swings in glucose levels. Over time, high blood sugar levels damage the small blood vessels in the kidneys, leading to CKD.
Even if you don’t have diabetes now, alcohol can increase your risk of developing type 2 diabetes, especially when combined with weight gain and a poor diet. That means you could be increasing your risk for two major kidney stressors—alcohol and blood sugar—at the same time.
Managing your alcohol intake is one of the most effective ways to protect your kidneys if you live with or are at risk for diabetes.
Can Your Kidneys Heal from Alcohol Damage?
Yes—sometimes. If caught early enough, kidney damage from alcohol may be reversible. Research shows that mild kidney issues can improve within just 4 weeks of alcohol abstinence.
However, the ability to recover depends on several factors:
-
How long and how heavily you’ve been drinking
-
Whether you have other conditions like diabetes, liver disease, or high blood pressure
-
The type of damage: AKI may heal with time, but CKD is usually permanent
If you're concerned about your kidney health, the best first step is to stop drinking or reduce your alcohol intake significantly. Then, schedule an appointment with a healthcare provider who can order the right tests and help you track your recovery.
Explore how to reduce proteinuria to support kidney recovery during detox and repair.
How Much Alcohol is Too Much for Your Kidneys?

The National Kidney Foundation and CDC recommend:
-
Women: No more than 1 drink/day, 7 per week
-
Men: No more than 2 drinks/day, 14 per week
But even this level may be too much for those with:
-
High blood pressure
-
Diabetes
-
Liver disease
-
A family history of CKD
Binge drinking, even occasionally, increases the risk of AKI and future CKD.
Tips to Protect Your Kidneys—Starting Today
You don’t have to wait for symptoms to take action. Try these steps:
-
Limit alcohol: No more than 1 drink/day (women), 2 (men)
-
Stay hydrated: Drink water with alcohol
-
Check your blood pressure regularly
-
Eat a kidney-friendly diet: Low sodium, fewer processed foods
-
Avoid binge drinking
-
Get regular checkups if you have any risk factors
Some people may need to avoid alcohol entirely—especially those with kidney, liver, or heart conditions.
Take Care of Your Kidneys Now
Your kidneys may not get as much attention as your heart or liver, but they’re just as essential. If you drink regularly, especially heavily, your kidneys could be working overtime without your knowledge.
Fortunately, you have the power to make changes. Recognizing the early signs of kidney damage and taking steps to reduce alcohol use can help protect your kidneys for years to come.
Want to Take Charge of Your Kidney Health?
Try Ribbon Checkup’s at-home kidney function test—a simple, reliable way to monitor your kidney health from home. For more on how habits like drinking affect your kidneys, explore our expert-backed blogs.
Related Resources
-
Does Alcohol Cause Kidney Stones?
Explore how alcohol contributes to dehydration and mineral imbalances that may lead to kidney stone formation. -
How to Tell If You're Dehydrated: Signs, Symptoms & Tests
Dehydration is one of the most immediate effects of alcohol on the kidneys. Learn how to recognize and test for it. -
How to Protect Your Kidneys? Kidney Health Guide
Practical strategies to reduce alcohol-related kidney damage and support long-term kidney health.
References
Drinking Alcohol Affects Your Kidneys. (2024, November 13). Retrieved June 6, 2025, from National Kidney Foundation website: https://www.kidney.org/news-stories/drinking-alcohol-affects-your-kidneys#:~:text=Heavy%20drinking%20doubles%20the%20risk,the%20body%2C%20leading%20to%20dehydration.
Epstein, M. (2025). Alcohol’s Impact on Kidney Function. Alcohol Health and Research World, 21(1), 84. Retrieved from https://pmc.ncbi.nlm.nih.gov/articles/PMC6826793
Heywood, A. L. (2025, January 30). Can People with Kidney Disease Drink Alcohol? Retrieved June 6, 2025, from Healthline website: https://www.healthline.com/health/kidney-disease/can-you-drink-alcohol-with-kidney-disease
How alcohol affects blood pressure. (2025). Retrieved June 6, 2025, from Mayo Clinic website: https://www.mayoclinic.org/diseases-conditions/high-blood-pressure/expert-answers/blood-pressure/faq-20058254
Joo, Y. S., Koh, H., Nam, K. H., Lee, S., Kim, J., Lee, C., … Han, S. H. (2020). Alcohol Consumption and Progression of Chronic Kidney Disease: Results From the Korean Cohort Study for Outcome in Patients with Chronic Kidney Disease. Mayo Clinic Proceedings, 95(2), 293–305. https://doi.org/10.1016/j.mayocp.2019.06.014
Perneger, T. V., Whelton, P. K., Puddey, I. B., & Klag, M. J. (1999). Risk of End-stage Renal Disease Associated with Alcohol Consumption. American Journal of Epidemiology, 150(12), 1275–1281. https://doi.org/10.1093/oxfordjournals.aje.a009958
Schaeffner, E., & Ritz, E. (2012). Alcohol and kidney damage: a Janus-faced relationship. Kidney International, 81(9), 816–818. https://doi.org/10.1038/ki.2012.14
Varga, Z. V., Matyas, C., Janos Paloczi, & Pacher, P. (2017). Alcohol Misuse and Kidney Injury: Epidemiological Evidence and Potential Mechanisms. Alcohol Research : Current Reviews, 38(2), 283. Retrieved from https://pmc.ncbi.nlm.nih.gov/articles/PMC5513691/?utm_source=chatgpt.com

Dr. Abel Tamirat is a licensed General Practitioner and ECFMG-certified international medical graduate with over three years of experience supporting U.S.-based telehealth and primary care practices. As a freelance medical writer and Virtual Clinical Support Specialist, he blends frontline clinical expertise with a passion for health technology and evidence-based content. He is also a contributor to Continuing Medical Education (CME) programs.


