Why Is My Fasting Blood Sugar High but My A1C Is Normal?
 Written By
Abel Tamirat, MD
Written By
Abel Tamirat, MD
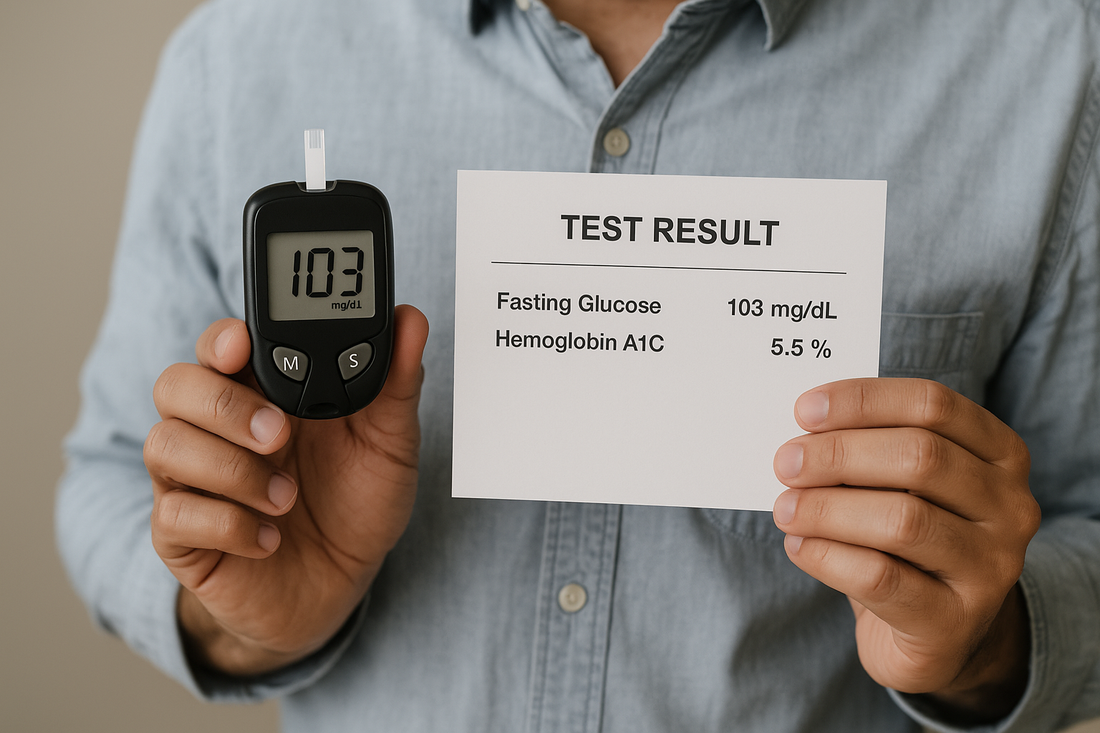
If your fasting blood sugar is over 100 mg/dL but your A1C is still normal, you’re probably wondering what’s going on.
Here’s the answer: This mismatch is common. It often means your body is starting to have trouble managing blood sugar—especially in the early stages of insulin resistance or metabolic issues. Your A1C might look fine, but your fasting numbers could be signaling a hidden problem.
This article explains why these numbers can be out of sync, what it means for your health, and what steps to take next.
What do A1C and fasting blood sugar actually measure?
These two tests check your blood sugar in different ways:
-
A1C shows your average blood sugar over the past 2 to 3 months.
-
Fasting blood sugar shows your blood sugar at a single moment, after not eating for at least 8 hours.
If your blood sugar tends to spike only in the morning—or only after certain meals—your average may still look normal on an A1C test. Learn more about how to monitor glucose levels at home to catch these variations.
Why can fasting blood sugar be high when your A1C is normal?
1. Dawn phenomenon
In the early morning, your body releases hormones like cortisol and growth hormone. These can raise your blood sugar naturally, even before you eat. This is called the dawn phenomenon.
People with insulin resistance or early-stage type 2 diabetes often see higher fasting numbers due to this.
2. Early insulin resistance
This is one of the most common causes of high fasting glucose. Your body starts having trouble using insulin well—especially overnight.
The result: your blood sugar stays high in the morning. But your A1C can still be in the normal range if your levels drop later in the day.
This condition is known as impaired fasting glucose (IFG) and is considered a type of prediabetes, is a form of prediabetes.
3. Red blood cell differences
A1C is based on how sugar sticks to your red blood cells. But if your body replaces these cells more often—or if you have certain blood traits—your A1C may look lower than it really should be.
Factors that can affect A1C:
-
Iron deficiency anemia
-
Kidney disease
-
Sickle cell trait or other hemoglobin variants
This is common in people with iron deficiency, kidney disease, or conditions like anemia and liver disease.
4. Post-meal spikes are being missed
If you don’t check your sugar after eating, you might be missing major spikes. These don’t always show up in fasting tests or in your A1C—but they still cause damage to your blood vessels and organs over time.
Tracking sugar 1 to 2 hours after eating—or using a continuous glucose monitor (CGM)—can reveal hidden highs.
You can use urine glucose test strips or a CGM to see hidden highs.
5. Lab or test inaccuracies
Even though A1C and fasting glucose are standard tests, there are still errors. In some cases, your A1C might be falsely low due to how the test was done or how your blood behaves. If this is suspected, a provider may suggest a fructosamine test or OGTT for a more accurate picture.
In these cases, doctors may recommend alternative tests like:
-
Fructosamine (shows average sugar over the past 2–3 weeks)
-
Oral glucose tolerance test (OGTT)
Should you be concerned?

Yes. High fasting blood sugar is a sign that your metabolism may be shifting—even if your A1C hasn’t changed yet.
A1C below 5.7% is considered normal. Between 5.7% and 6.4% is in the prediabetes range. An A1C of 6.5% or higher indicates diabetes.
For fasting blood sugar, anything below 100 mg/dL is normal. Readings between 100 and 125 mg/dL are considered prediabetes. A result of 126 mg/dL or higher may point to diabetes.
So, if your fasting sugar falls between 100 and 125 mg/dL—even with a normal A1C—it’s still considered prediabetes.
To assess risk further, explore type 1 diabetes life expectancy and diabetes and swollen feet, which are common complications in later stages.
What steps should you take?

1. Track your blood sugar
You don’t need to test constantly, but try these points:
-
Fasting (morning)
-
1–2 hours after meals
-
Bedtime
This will help you understand your body’s patterns.
This will help you understand your body’s patterns. You can also use an at-home blood sugar test kit to monitor trends.
2. Ask your doctor about more tests
If your numbers are consistently high, bring it up with your provider. They may suggest:
-
A glucose tolerance test (OGTT)
-
Insulin and C-peptide testing
-
A continuous glucose monitor (CGM)
-
Fructosamine test (if A1C seems unreliable)
They may also look at factors like iron levels, kidney function, or hemoglobin variants that can skew A1C.
3. Make targeted lifestyle changes
Research shows that even small steps can lower fasting glucose and improve insulin sensitivity.
Proven strategies include:
-
Losing 5–7% of body weight (if applicable)
-
Eating fewer refined carbs, more fiber and protein
-
Walking for 10–15 minutes after meals
-
Avoiding late-night eating
-
Strength training or resistance exercise
A 2023 meta-analysis published in The Lancet Diabetes & Endocrinology confirmed that these habits significantly reduce fasting glucose—even without medication.
How is this linked to liver health?

Your liver helps regulate blood sugar—especially during fasting periods.
When your liver releases too much glucose overnight, your fasting sugar goes up. This often happens in people with non-alcoholic fatty liver disease (NAFLD).
Improving liver health through nutrition, exercise, and reduced sugar intake can directly help your blood sugar stay more stable.
What’s the takeaway?
If your fasting blood sugar is high but your A1C is normal, it’s not something to ignore. It often means your body is starting to struggle with blood sugar regulation.
This mismatch may signal early insulin resistance, where your body isn’t responding well to insulin during fasting. It could also be caused by the dawn phenomenon, a natural rise in blood sugar that happens in the early morning. In some cases, red blood cell turnover can affect how your A1C is measured, making it appear lower than it should. Or you may be having blood sugar spikes after meals that aren’t being detected.
Order your Ribbon Checkup test today and catch early signs before they become serious health issues.
Related Resources
-
How to Monitor Glucose Levels at Home
Learn how to track daily sugar fluctuations—especially those missed by A1C tests. -
Blood Sugar Test Kit: A Complete Guide
Discover how to choose and use the right tools for monitoring fasting and post-meal glucose. -
Type 4 Diabetes: Understanding Age-Related Insulin Resistance
Explore how aging impacts blood sugar, insulin sensitivity, and early warning signs.
References
A Goday, Bellido, D., I Sajoux, Crujeiras, A. B., B Burguera, García-Luna, P. P., … Casanueva, F. F. (2016). Short-term safety, tolerability and efficacy of a very low-calorie-ketogenic diet interventional weight loss program versus hypocaloric diet in patients with type 2 diabetes mellitus. Nutrition and Diabetes, 6(9), e230–e230. https://doi.org/10.1038/nutd.2016.36
and, D. (2024, December 30). National Institute of Diabetes and Digestive and Kidney Diseases. Retrieved August 5, 2025, from National Institute of Diabetes and Digestive and Kidney Diseases website: https://www.niddk.nih.gov/
Davies, M. J., Aroda, V. R., Collins, B. S., Gabbay, R. A., Green, J., Maruthur, N. M., … Buse, J. B. (2022). Management of Hyperglycemia in Type 2 Diabetes, 2022. A Consensus Report by the American Diabetes Association (ADA) and the European Association for the Study of Diabetes (EASD). Diabetes Care, 45(11), 2753–2786. https://doi.org/10.2337/dci22-0034
Diabetes Overview. (2023, September 8). Diabetes: What It Is, Causes, Symptoms, Treatment & Types. Retrieved August 5, 2025, from Cleveland Clinic website: https://my.clevelandclinic.org/health/diseases/7104-diabetes
Hemoglobin A1C (HbA1c) Test. (2025). Retrieved August 5, 2025, from Medlineplus.gov website: https://medlineplus.gov/lab-tests/hemoglobin-a1c-hba1c-test/
Rohit Loomba, & Sanyal, A. J. (2013). The global NAFLD epidemic. Nature Reviews Gastroenterology & Hepatology, 10(11), 686–690. https://doi.org/10.1038/nrgastro.2013.171
World. (2024, November 14). Diabetes. Retrieved August 5, 2025, from Who.int website: https://www.who.int/news-room/fact-sheets/detail/diabetes
Zeitler, P. S., Hirst, K., Pyle, L., Linder, B., Copeland, K., Arslanian, S. A., … Kaufman, F. R. (2012). A Clinical Trial to Maintain Glycemic Control in Youth with Type 2 Diabetes. New England Journal of Medicine, 366(24), 2247–2256. https://doi.org/10.1056/nejmoa1109333

Dr. Abel Tamirat is a licensed General Practitioner and ECFMG-certified international medical graduate with over three years of experience supporting U.S.-based telehealth and primary care practices. As a freelance medical writer and Virtual Clinical Support Specialist, he blends frontline clinical expertise with a passion for health technology and evidence-based content. He is also a contributor to Continuing Medical Education (CME) programs.


